A 66-year-old male ex-smoker with hypertension, type 2 diabetes mellitus and dyslipidaemia was admitted due to a non-ST segment elevation myocardial infarction. The catheterisation depicted an extensive and calcified disease: chronic total obstruction of the right coronary and severe disease with a giant aneurysm at the first marginal branch as the culprit vessel. After discussion, the right coronary was treated before the circumflex-giant aneurysm was closed with a stent graft and its multiple severe stenosis solved with two drug-eluting stents. We provide a multimodality approach for a complex case and briefly discuss the available options.
Um homem de 66 anos, ex-fumador, hipertenso, com diabetes tipo II e dislipidemia, foi admitido por enfarte do miocárdio sem supradesnivelamento de ST. O cateterismo revelou doença extensa e calcificada: oclusão crónica e total da artéria coronária direita e doença severa com aneurisma gigante da primeira obtusa marginal, como lesão alvo. Após discussão, foi tratada a artéria coronária direita e posteriormente foi encerrado o aneurisma gigante de circunflexa com um stent e as suas múltiplas estenoses severas foram resolvidas com dois stents com fármaco. Providenciamos uma abordagem multimodal para um caso complexo e discutimos brevemente as diferentes opções possíveis.
Coronary artery aneurysm is defined as a coronary dilatation which exceeds the diameter of normal adjacent segments or the diameter of the patient's largest coronary vessel by 1.5 times. A giant coronary aneurysm is usually defined as a dilatation which exceeds the diameter of normal adjacent segments or the diameter of the patient's largest coronary vessel by 4 times. Described by Bourgon1, it is a rare disease which has been diagnosed with increasing frequency since the advent of coronary angiography2,3. The incidence has been deemed to vary from 1.5% to 5% with male dominance and a predilection for the right coronary artery2,3.
With several unanswered questions, coronary aneurysms are managed in several ways (conservative, stenting or cardiac surgery)4–6. Here, we present a case with a giant coronary aneurysm in a culprit vessel in an acute coronary syndrome setting.
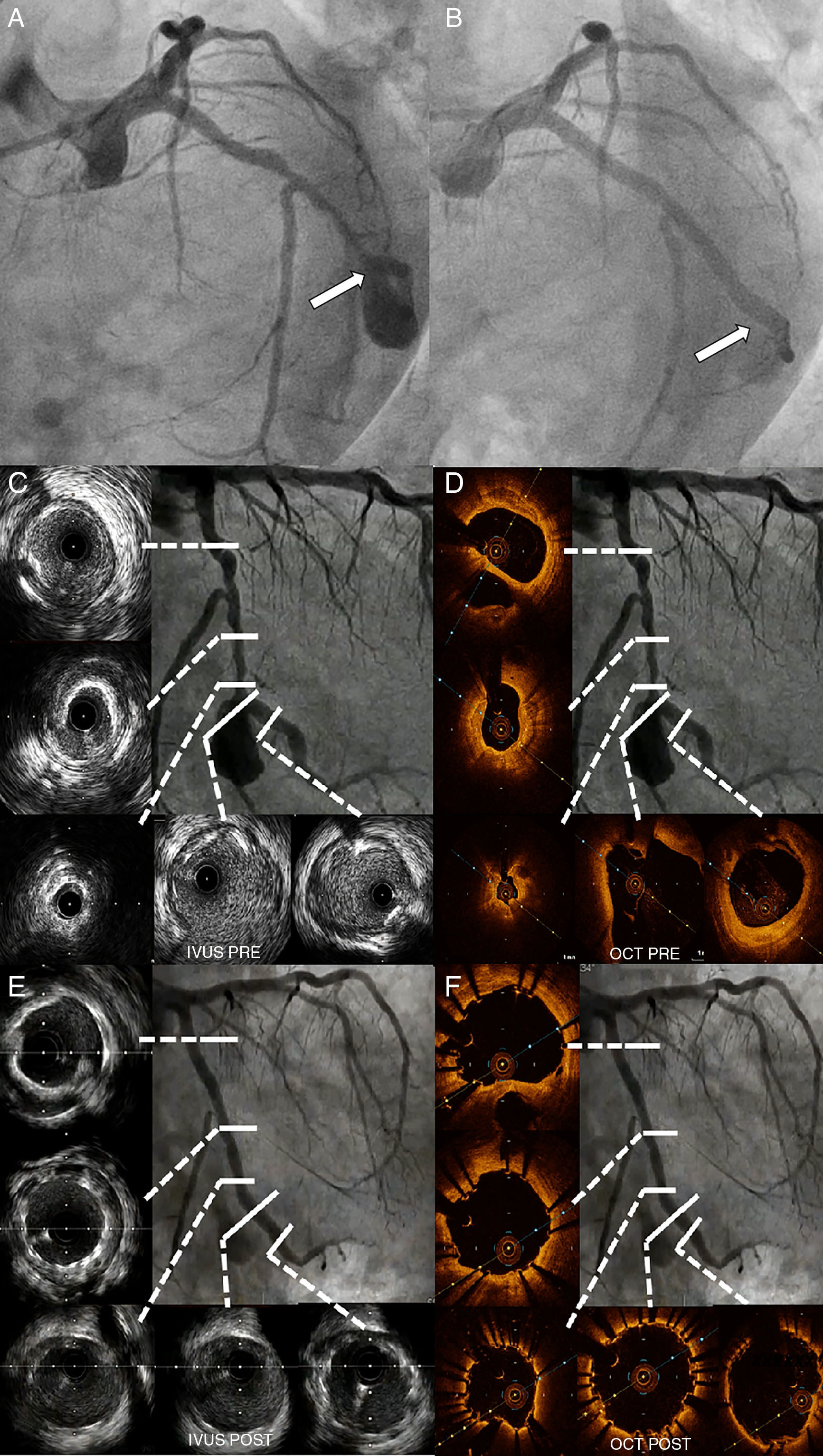
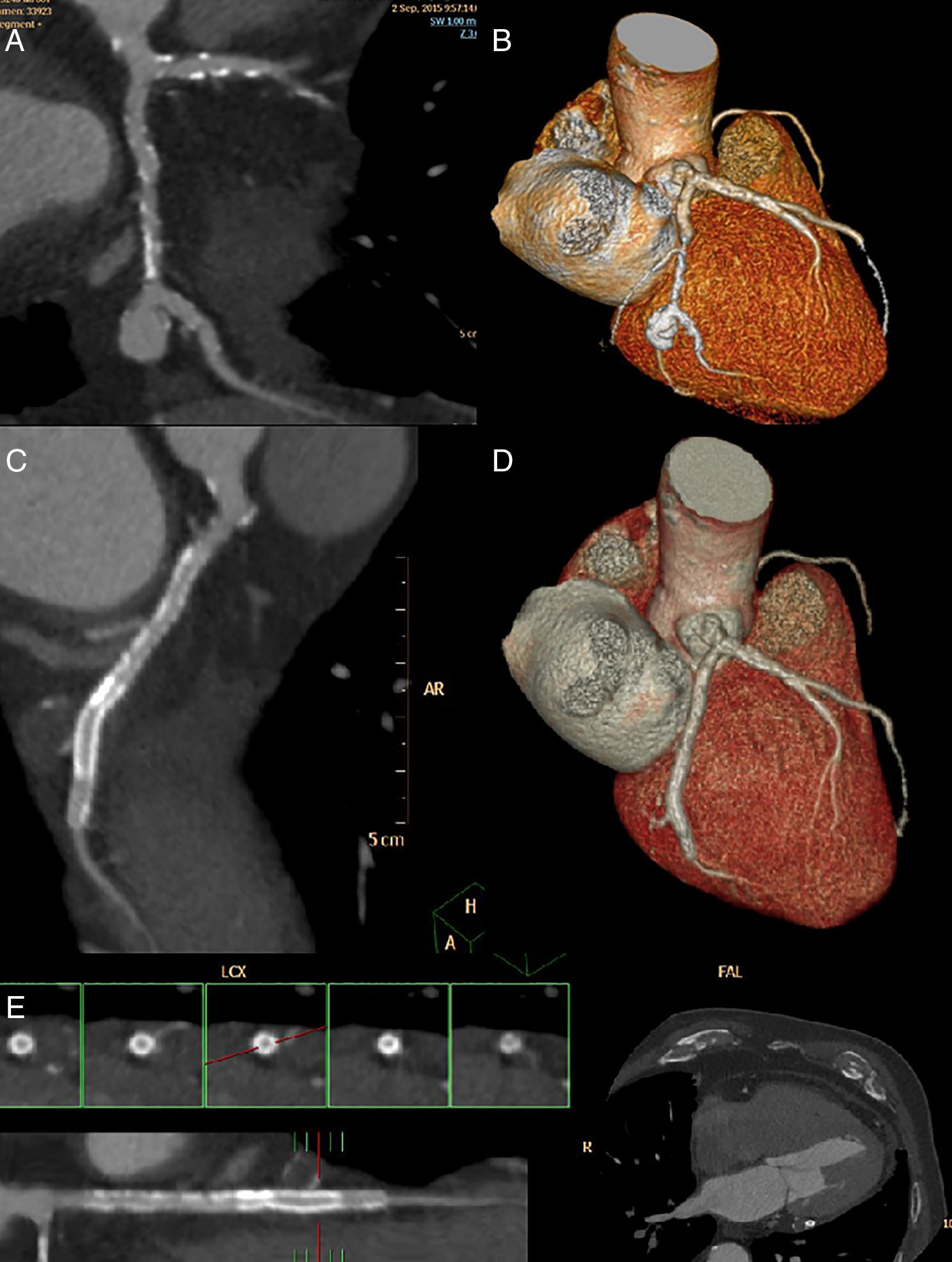
Case ReportA 66-year-old male ex-smoker with hypertension, type 2 diabetes mellitus and dyslipidaemia, without history of trauma, vasculitis or connective tissue disorders, was admitted due to a non-ST segment elevation myocardial infarction with mild troponin I elevation (Grace 2.0: 93; estimated 1-year mortality 3.1%; estimated 3-year mortality: 7.1%; Crusade: 27, 6.1% bleeding risk). The ECG showed sinus rhythm with lateral negative T waves, a transthoracic echocardiogram revealed normal left ventricular ejection fraction and the cardiac catheterisation depicted an extensive and calcified coronary disease, including a chronic total obstruction at the proximal segment of the right coronary artery together with a severe and diffuse disease with a giant aneurysm at the first obtuse marginal branch as the culprit lesion (Figure 1A), TIMI flow III. The left anterior descending artery revealed no significant stenosis. Since the patient remained stable on medical treatment, we decided further study was necessary and a coronary CT was ordered, confirming the previous findings (Figure 2A-B) and highlighting a giant saccular coronary aneurysm (17x14mm) with a wide neck at a big obtuse marginal level.
Coronary CT scan aneurysm characterisation. A) LCx maximum pixel intensity multiplanar reconstruction or MIP-MPR. B). Cardiac 3D volume rendering oriented like cranial RAO showing LCx and aneurysm. C) 3-month-follow-up coronary CT scan. LCx centreline curved multiplanar reconstruction. D) LCx 3D rendering. E) LCX straight line reconstruction derived from curved centreline. MPR (so called virtual IVUS). Axial images (red mark) revealing the stent.
Thus, the following treatment options were considered to treat the patient: coronary artery bypass grafting (CABG), coil embolisation or stent implantation (covered). CABG was discarded because the left anterior descending artery was free of severe disease and the less-invasive interventional approach was preferred by the patient and his family. Treatment dilemmas at this point were:
- •
Right coronary artery chronic total occlusion.
- •
Technical difficulty in closing the aneurysm, with a small branch arising from its neck.
- •
Wide neck posing some issues regarding the use of coils, together with severe, calcified and diffuse lesions before the aneurysm.
Thus, we decided on the “covered or graft” stent option. First, we performed the interventional procedure on the right coronary artery chronic total occlusion. Using a regular anterograde approach, 2 drug-eluting stents (DES) were successfully implanted. Later on, we selected the Papyrus® stent (Biotronik, Germany), a single layer covered (90μm polyurethane porous layer) stent based on the Orsiro/Prokinetic platform, which is supposed to achieve a greater bending flexibility and deliverability, and is designed to treat coronary perforations.
Then, intracoronary imaging (IVUS, Boston-Scientific, MA, USA; Figure 1C and OCT, St Jude, St. Paul, Minn., USA; Figure 1D), was performed, depicting a severely diseased and calcified vessel, with a tight calcified stenosis (ALM:1.78cm2), previous to the neck of the aneurysm. A first attempt to cross the graft directly failed, probably because of marked tortuosity. The whole vessel was consecutively predilated with a 2.5x12mm balloon. A mother-and-child system was then advanced (6F-Guideliner, Vascular Solutions Inc., Minn., USA), allowing to cross the lesion with the stent-graft (3.5x20mm) and its proper positioning (14atm). Later, two DES were consecutively implanted, covering all the LCx stenosis, including the stent graft, with a good angiographic outcome and complete aneurysm obliteration, Figure 1B. In addition, implanting a DES inside the stent-graft could hopefully potentially diminish the proliferative/thrombotic trend described for these covered scaffolds.
The result was optimised with several high pressure 3.5x15mm noncompliant balloon inflations, with a good angiographic outcome. This was double-checked with intracoronary imaging (IVUS; Figure 1E and IVUS; Figure 1F).
The patient remained free from angina and was discharged 48hours post-intervention, with an asymptomatic mild troponin increase due to the (deliberate) closure of the small branch located near the aneurysm's neck. A 3-month follow-up coronary CT-scan showed the persistence of the good outcome, with complete aneurysm closure (Figure 2C-E). The patient was discharged on aspirin and ticagrelor (12 months). At 12-month follow-up the patient was in NYHA functional class I without angina, and the control angiogram confirmed the stents’ patency.
DiscussionAlthough several causes have been reported, atherosclerosis is the most prevalent, accounting for more than 50% of coronary aneurysms in adults. Reported complications include thrombosis and distal embolisation, rupture and vasospasm, causing ischaemia, heart failure, arrhythmias and, less frequently, compression of surrounding structures and fistulisation into one of the cardiac chambers. In addition, controversy persists regarding the use of medical management (antithrombotic) or interventional/surgical procedures1–8. Sometimes, the aneurysm concept is confused or mixed with “ectasia”. The term ‘ectasia’ refers to a diffuse dilation of a coronary artery, while focal dilation is properly called ‘coronary aneurysm’9. This condition has been suggested as a variant of coronary atherosclerosis10.
Occasionally, the clinical presentation is acute, like in our case. Consequently, we need to have, in advance, detailed protocols and guidelines in these cases warranting prompt and quick management. Interventional cardiology advances, with new techniques and devices, such as in our case, are beginning to make less-invasive treatment feasible for complex patients with aneurysms. The new intracoronary imaging techniques provide a unique opportunity to guide and improve our interventional procedures. In our case, we decided to opt for the multivessel interventional option because the left anterior descending artery was free of severe disease, and we used both IVUS and OCT for academic purposes.
Nevertheless, the natural history and long-term prognosis remains obscure, since definitive data are scarce. Therefore, until we have the results of the currently ongoing international registry on coronary artery aneurysm (CAAR, ClinicalTrials.gov Identifier: NCT02563626), we can only adopt an empirical approach, based on small series or case reports.
ConclusionHere, we propose an alternative to simply manage a potentially complex condition from an interventional point of view in an acute setting guided by the unique contribution of intracoronary imaging.
Conflicts of interestThe authors have no conflicts of interest to declare.