Exercise-induced cardiac remodeling is frequent in athletes. This adaptation is structurally manifested by an increase in cardiac dimensions and mass. Soldiers are also subject to intense physical exercise, although with different characteristics.
ObjectiveTo compare exercise-induced cardiac remodeling in competitive athletes and in soldiers on a special forces training course.
MethodsWe studied 17 soldiers (all male and Caucasian, mean age 21±3 years) who completed a special forces course and 17 basketball players (47.3% male, 64.7% Caucasian, mean age 21±3 years). Assessment included a transthoracic echocardiogram and analysis of myocardial mechanics. This assessment was performed at the beginning and end of the military course and the sports season, respectively.
ResultsCardiac remodeling was observed in both groups. The soldiers presented a predominantly eccentric pattern, with increased left ventricular (LV) size (49.7±3.2 vs. 52.8±3.4 mm; p<0.01), increased LV mass (93.1±7.7 vs. 100.2±11.4 g/m2; p<0.01) and decreased relative wall thickness (0.40±0.1 vs. 0.36±0.1; p=0.05). The basketball players showed a concentric pattern, with decreased LV size (52.0±4.7 vs. 50.4±4.7 mm; p=0.05), and increased relative wall thickness (0.33±0.1 vs. 0.36±0.1; p=0.05). Although there was no significant difference in LV myocardial strain in the groups separately, when compared there was a significant decrease (-20.2±1.6% vs. -19.4±2.1%; p=0.03).
ConclusionCardiac remodeling was frequent, with an eccentric pattern in soldiers and a concentric pattern in basketball players. Myocardial deformation may represent a physiological adaptation to physical exercise.
A remodelagem cardíaca induzida pelo exercício físico é frequente em atletas. Esta adaptação manifesta-se a nível estrutural com o aumento das dimensões e massa cardíacas. Os militares também são sujeitos a exercício físico intenso, com especificidades distintas.
ObjetivoComparar a remodelagem cardíaca induzida pelo exercício físico em atletas de competição e pelo treino militar em militares a frequentar um curso de forças especiais.
MetodologiaEstudámos 17 militares (género masculino e caucasianos, idade média 21 ± 3 anos) que ingressaram no curso de Comandos e 17 basquetebolistas (47,3% do género masculino, 64,7% caucasianos, idade média 21 ± 3 anos). A avaliação incluiu um ecocardiograma transtorácico com análise da mecânica miocárdica. Esta avaliação foi realizada no início e no final do curso militar e da época desportiva, respetivamente.
ResultadosA remodelagem cardíaca teve características distintas: os militares apresentaram um padrão predominantemente excêntrico, com aumento das dimensões do ventrículo esquerdo (49,7 ± 3,2 versus 52,8 ± 3,4 mm; p < 0,01) e da massa (93,1 ± 7,7 versus 100,2 ± 11,4 g/m2; p < 0,01) e diminuição da espessura relativa das paredes (0,40 ± 0,1 versus 0,36 ± 0,1; p = 0,05); os basquetebolistas apresentaram um padrão concêntrico, com diminuição das dimensões do ventrículo esquerdo (52,0 ± 4,7 versus 50,4 ± 4,7 mm; p = 0,05) e da espessura relativa das paredes (0,33 ± 0,1 versus 0,36 ± 0,1; p = 0,05). Apesar da deformação miocárdica global do ventrículo esquerdo não apresentar diferenças significativas entre os grupos, quando analisados em conjunto o seu valor diminuiu (-20,2 ± 1,6% versus -19,4 ± 2,1%; p = 0,03).
ConclusãoA remodelagem cardíaca foi frequente, com padrão excêntrico nos militares e concêntrico nos atletas. A mecânica miocárdica poderá representar uma adaptação fisiológica induzida pelo exercício físico.
body mass index
blood pressure
diastolic blood pressure
electrocardiogram
fat mass
global longitudinal strain
heart rate
interventricular septum
left atrial
left ventricular
left ventricular end-diastolic diameter
left ventricular ejection fraction
left ventricular end-systolic diameter
muscle mass
relative wall thickness
systolic blood pressure
tricuspid annular plane systolic excursion
transthoracic echocardiography
difference
Intense and prolonged physical exercise leads to changes in cardiovascular physiology known as ‘athlete's heart’. Chief among these alterations are increased cardiac size, volumes and mass and improved functional parameters, particularly diastolic function.1 Classically, two forms of cardiac remodeling have been described: concentric remodeling associated with static exercise, and eccentric remodeling associated with dynamic exercise.2 For example, marathon runners present eccentric remodeling due to volume overload resulting from increased cardiac output, while weightlifters show concentric remodeling due to pressure overload.3 It should be noted that this distinction is not absolute, since most sports involve both static and dynamic exercise, and hence lead to mixed remodeling.4
However, athletes are not the only individuals who undergo high-intensity training. Soldiers, especially in the special forces, also undergo physically demanding training that involves various forms of both static and dynamic exercise. Overall, the volume of exercise required of these soldiers can be compared to that of competitive athletes, and may often be even higher. However, military training is unique with regard to the methodologies used and the influence of other variables arising from military life.5
The manifestations of exercise-induced cardiac remodeling can overlap with those of pathological conditions, especially cardiomyopathy, and differential diagnosis is often challenging.6 In this context, pre-participation screening of athletes and interpretation of diagnostic exams in this population are of great importance. In the last decade, new imaging techniques have been developed that enable detailed myocardial assessment, such as analysis of myocardial mechanics by transthoracic echocardiography (TTE).7
The main aim of this study was to characterize and compare cardiac remodeling in professional basketball players over the course of a season and in soldiers on a special forces course.
MethodsThis observational, longitudinal, case-control study assessed special forces soldiers and competitive athletes at the beginning and end of a military training course and a sports season, respectively. Male and female individuals between the ages of 18 and 35 years were included. The soldiers were selected from those who enrolled in a Portuguese Army commando course and were assessed between January and June 2016. The athletes belonged to two professional basketball teams, one men's and the other women's, competing in the national men's Division 1 and the national women's league, respectively, and were assessed in October 2015 and March/April 2016. Thus, both groups were assessed over a period of about six months. The group of soldiers consisted of the 17 out of 76 trainees (54 dropouts, approximately 70% of trainees) who successfully completed the course and met the inclusion criteria. All of these soldiers had previously participated in competitive sports. The athlete population was composed of 17 basketball players, eight male and nine female.
All of the study subjects were volunteers and gave their informed consent to participate in the study. The protocol was approved by the Ethics Committee of the Medical School of the University of Coimbra (reference protocol 087/2015).
Characteristics of physical exercise in the study populationThe commando course involves high-intensity physical exercise intended to develop aerobic and anaerobic capacity. To this end, the soldiers undergo dynamic and static physical training, including various sports including running, swimming, gymnastics and weightlifting. In addition, they undergo military physical training, which aims to instill and develop psychomotor techniques and abilities that enable soldiers to perform their duties under adverse conditions. This physical training involves obstacle courses, intense running interspersed with marching, carrying loads, and similar activities. The training program is divided into two stages: the first stage consists of 10 weeks of vigorous-intensity physical exercise (77-95% of maximum heart rate [HR]),8 five times per week with a mean duration of four hours per day, while the second phase consists of 15 weeks of vigorous-intensity physical exercise (77-95% of maximum HR) interspersed with periods of near maximal- or maximal-intensity exercise (≥96% of maximum HR),8 five times per week for a mean of four hours per day. In addition to this scheduled training, the soldiers are under constant physical, psychological and emotional strain, which is difficult to quantify.
Basketball involves numerous movements that require speed, skill and strength and involve dynamic and static exercise, with a general component and a specific component. The general component is provided by continuous running at speed and with changes in direction, and gymnastic and flexibility exercises. The specific component consists mainly of training in coordination by learning and practicing technical maneuvers. The players train four times a week and play one game a week. The mean duration of each training session is three hours, divided into three separate periods: warmup, basketball training with general and specific exercises, and cooldown. The players are subject to periods of vigorous- to near maximal-intensity exercise, with other periods of low- to moderate-intensity exercise. Overall, the training sessions for these athletes can be classified as vigorous-intensity (77-95% maximum HR).8
Clinical assessmentAll participants underwent a full physical examination and thorough collection of medical history, performed by a sports medicine physician or a cardiologist. Emphasis was placed on cardiovascular risk factors, dietary habits, medications, and sports history, including the number of hours of training and of sleep during the course or season.
Anthropometric assessmentThe anthropometric assessment was performed by a nurse and a health technician. Height was measured using a tape measure, and weight, percentage fat mass (FM) and muscle mass (MM) were measured using a digital full-body composition monitor (Omron® HBF-510W) using bioelectrical impedance. Systolic blood pressure (SBP), diastolic blood pressure (DBP) and HR were assessed using an upper arm blood pressure (BP) monitor (Omron® HEM-7113), in accordance with current guidelines.9 Changes (Δ) in variables (weight, MM, FM, SBP, and DBP) were calculated according to the following formula: (final value - initial value)/initial value×100.
Electrocardiographic assessmentAll individuals underwent a 12-lead electrocardiogram (ECG) (Norav® 1200HR), analyzed by two cardiologists and interpreted according to the ‘refined’ criteria.10
Echocardiographic assessmentAll transthoracic echocardiograms were performed by a cardiologist with a Vivid 7 ultrasound system (GE Healthcare®), and included the various echocardiographic views and techniques recommended by the European Society of Cardiology (two-dimensional; M-mode; color, pulsed wave, continuous wave and tissue Doppler; and myocardial strain assessed by speckle tracking).11
Wall thickness and left ventricular (LV) dimensions were measured via parasternal long-axis view. Relative wall thickness (RWT) was calculated using the formula (2×LV posterior wall thickness/LV end-diastolic diameter [LVEDD]) and LV mass was calculated using the Devereux formula.12 LV volume and left atrial (LA) volume were determined using the modified Simpson's rule, with images obtained in apical 4- and 2-chamber views. The LA volume index was obtained by indexing to body surface area. LV ejection fraction (LVEF) was determined using Simpson's method. Pulsed wave Doppler was acquired in apical 4-chamber view, and peak E and A wave velocities and E/A ratio were measured. Tissue Doppler images of the mitral and tricuspid annuli were obtained to measure the E and E′ waves, and to measure S′ wave velocities, respectively. Tricuspid annular plane systolic excursion (TAPSE) was determined by M-mode. Speckle tracking was used to calculate LV global longitudinal strain (GLS) using images from apical 4-, 2- and 3-chamber views and an 18-segment model. Cardiac cycles were acquired during the same respiratory phase (exhalation). Three consecutive cycles were recorded and mean sinus rhythm was calculated with a frame rate >60 frames per second. The quality of the exam was considered good when no more than two segments were excluded, and excellent when all segments were analyzed.
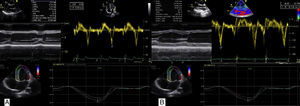
Figure 1 shows examples of TTE of a soldier and of an athlete after the course or season, respectively.
(A) Transthoracic echocardiographic images of a soldier following the special forces course, showing no left ventricular (LV) wall thickening and LV end-diastolic diameter near the upper normal limit, above-normal diastolic function parameters and normal global longitudinal strain (GLS) values; (B) transthoracic echocardiographic images of a basketball player after the sports season, with LV wall thickening near the upper normal limit and normal diastolic function parameters and GLS.
Categorical variables were presented as frequency and percentage, and compared with the chi-square and Fisher's tests as appropriate. The Kolmogorov-Smirnov test was used to test continuous variables for normality of distribution. Variables with a normal distribution were expressed as mean and standard deviation, and the Student's t test was used for group comparisons. Levene's test was used to assess the homogeneity of variance of individual variables. Variables with a non-normal distribution were expressed as median and interquartile range, and the groups were compared using the Mann-Whitney and Kruskal-Wallis tests. Pearson's correlation was used to analyze associations between MM and FM and echocardiographic parameters. For all comparisons, a p-value <0.05 was considered statistically significant with a 95% confidence interval. All data were calculated and analyzed using SPSS version 20 (IBM SPSS® Inc., Chicago, IL, USA).
ResultsPopulation characteristicsThe characteristics of the study population are shown in Table 1. Briefly, the mean age of the two groups was similar, but there were significant differences in terms of gender and race. The soldiers played competitive sports for less time and had a higher body mass index. During the study period, the soldiers completed more hours of scheduled exercise per day and had fewer hours of sleep and fewer meals. Nearly a quarter of the population (20.6%) had at least one cardiovascular risk factor, of which smoking was the most common and was exclusive to the soldiers (17.6%), followed by dyslipidemia, which was also more common in the soldiers (5.9% vs. 2.9%, p=0.32). The study population had no family history of cardiovascular disease, hypertension or diabetes.
Baseline characteristics of the study population.
| Soldiers (n=17) | Basketball players (n=17) | p | |
|---|---|---|---|
| Demographic | |||
| Age (years) | 21±3 | 21±3 | 0.71 |
| Male (%) | 17/17 (100) | 8/17 (47.1) | <0.01 |
| Caucasian (%) | 17/17 (100) | 11/17 (64.7) | <0.01 |
| Anthropometric | |||
| BMI (kg/m2) | 25.3±2.7 | 23.1±2.7 | 0.03 |
| FM (%) | 19.1±3.3 | 25.1±12.1 | 0.56 |
| MM (%) | 41.3±2.1 | 35.0±7.8 | 0.09 |
| SBP (mmHg) | 128±10 | 131±13 | 0.35 |
| DBP (mmHg) | 73±7 | 64±13 | 0.90 |
| HR (bpm) | 65±12 | 73±7 | 0.81 |
| Sports history | |||
| Years of competition | 7.4±3.4 | 10.4±5 | 0.04 |
| Hours of training per day (course/season) | 4.0±0.5 | 2.9±1.1 | <0.01 |
| Hours of sleep per day (course/season) | 5.5±0.5 | 7.4±0.8 | <0.01 |
| Number of meals per day (course/season) | 4.0±1.0 | 4.7±1.0 | <0.01 |
BMI: body mass index; DBP: diastolic blood pressure; FM: fat mass; HR: heart rate; MM: muscle mass; SBP: systolic blood pressure.
The soldiers experienced significant weight gain, with increased MM, and more marked decreases in FM, SBP, DBP and HR than the basketball players (Table 2). The increase in MM and decrease in FM were seen in all male subjects.
Changes in anthropometric data.
| Soldiers (n=17) | Basketball players (n=17) | |||||
|---|---|---|---|---|---|---|
| Initial | Final | p | Initial | Final | p | |
| Weight (kg) | 75.2±7.8 | 77.4±6.6 | <0.01 | 76.7 | 76.3 | 0.63 |
| MM (%) | 41.3±2.1 | 44.4±1.8 | <0.01 | 35.0±7.8 | 35.6±7.5 | <0.01 |
| FM (%) | 19.1±3.3 | 13.1±3.5 | <0.01 | 25.1±12.1 | 24.9±11.6 | 0.88 |
| SBP (mmHg) | 128±10 | 122±7 | <0.01 | 132±13 | 133±12 | 0.54 |
| DBP (mmHg) | 73±7 | 66±5 | <0.01 | 73±7 | 74±9 | 0.64 |
| HR (bpm) | 66±12 | 59±6 | <0.01 | 65±13 | 61±11 | 0.19 |
DBP: diastolic blood pressure; FM: fat mass; HR: heart rate; MM: muscle mass; SBP: systolic blood pressure.
The percentage difference between the two groups in the changes in anthropometric data was statistically significant for weight, SBP, DBP, MM and FM (Figure 2). Unlike the basketball players, the soldiers gained weight (3.1±3.3 vs. -0.2±3.2%; p<0.01), with an increase in MM (7.5±4.1 vs. 1.7 ±2.4%; p<0.01) and greater decrease in FM (-31.4±15.7 vs. -0.8±14.9%; p<0.01). The soldiers experienced reductions in SBP (-4.8±3.0 vs. 1.4±7.4%; p<0.01) and DBP (-8.6±7.4 vs. 1.5±10.5%; p<0.01).
Electrocardiographic assessmentAll ECGs showed sinus rhythm and were considered normal or with only physiological alterations. The most common physiological alteration was sinus bradycardia (41.2%), followed by early repolarization (29.4%), LV hypertrophy (20.6%), incomplete right bundle branch block (11.8%), and first-degree atrioventricular block (2.9%).
Echocardiographic assessmentTTE revealed different structural patterns of cardiac remodeling (Table 3). In the soldiers, there was an increase in left chamber size, of both the left ventricle (49.7±3.2 vs. 52.8±3.4 mm; p<0.01) and the left atrium (63.4±10.5 vs. 71.2±12.1 ml; p=0.02), and a decrease in RWT (0.40±0.1 vs. 0.36±0.1; p=0.05). In the athletes, LV size decreased (52.0±4.7 vs. 50.4±4.7 mm; p=0.05), and interventricular septum (IVS) thickness (8.3±1.5 vs. 9.1±1.5 mm; p=0.03) and RWT (0.33±0.1 vs. 0.36±0.1; p=0.05) both increased. With regard to functional parameters, there was a reduction in resting LVEF in the soldiers (60±6 vs. 55±6%; p<0.01), and an increase in the S′ wave in both the soldiers (15±2 vs. 17±2 cm/s; p<0.01) and the basketball players (13±2 vs. 14±2 cm/s; p<0.01).
Changes in echocardiographic parameters.
| Soldiers (n=17) | Basketball players (n=17) | |||||
|---|---|---|---|---|---|---|
| Initial | Final | p | Initial | Final | p | |
| IVS (mm) | 9.7±1.0 | 9.9±1.0 | 0.39 | 8.3±1.5 | 9.1±1.5 | 0.03 |
| PW (mm) | 9.7±0.9 | 9.6±0.8 | 0.39 | 8.5±1.3 | 9.2±1.1 | 0.06 |
| LVMI (g/m2) | 93.1±7.7 | 100.2±11.4 | <0.01 | 82.3±15.9 | 87.1±18.4 | 0.18 |
| RWT | 0.40±0.1 | 0.36±0.1 | 0.05 | 0.33±0.1 | 0.37±0.1 | 0.03 |
| LVEDD (mm) | 49.7±3.2 | 52.8±3.4 | <0.01 | 52.0±4.7 | 50.4±4.7 | 0.05 |
| LVESD (mm) | 33.2±3.3 | 35.1±2.6 | 0.04 | 34.6±3.9 | 34.1±3.6 | 0.47 |
| LA volume (ml) | 63.4±10.5 | 71.2±12.1 | 0.02 | 54.1±10.0 | 56.6±11.6 | 0.29 |
| LVEF (%) | 60±6 | 55±6 | <0.01 | 58±5 | 58±6 | 0.15 |
| Lateral E′ (cm/s) | 19±3 | 19±3 | 0.92 | 18±3 | 17±4 | 0.18 |
| E/E′ | 5.3±1.0 | 5.3±0.9 | 0.61 | 5.1±1.3 | 5.6±0.7 | 0.14 |
| S′ (cm/s) | 15±2 | 17±2 | <0.01 | 13±2 | 14±2 | <0.01 |
| TAPSE (mm) | 25±4 | 26±5 | 0.34 | 24±3 | 25±3 | 0.41 |
| GLS (%) | -21.3±0.9 | -20.5±1.9 | 0.11 | -19.0±1.2 | -18.3±1.2 | 0.15 |
GLS: global longitudinal strain; IVS: intraventricular septum thickness; LA: left atrial; LVEDD: left ventricular end-diastolic diameter; LVEF: left ventricular ejection fraction; LVMI: left ventricular mass index; LVESD: left ventricular end-systolic diameter; PW: posterior wall; RWT: relative wall thickness; TAPSE: tricuspid annular plane systolic excursion.
When male participants were assessed separately, the different types of remodeling described above applied, with significant differences in LA volume (51.8±8.1 vs. 58.4±10.9 ml; p=0.05) and GLS (-19.4±1.3 vs. -17.6±1.7%; p=0.03) in the basketball players. Although there were no significant differences in GLS in the two groups at the beginning and end of the course or season, there was a significant difference when the two groups were compared (-20.2±1.6% vs. -19.4±2.1%; p=0.03). The echocardiographic findings in the two groups demonstrated differences in LVEDD, RWT, LVEF and S′ wave (Figure 3). Alterations in RWT and LVEDD were opposite: for the soldiers, RWT decreased (-10.0±14.3% vs. 12.1±22.5%; p<0.01) and LVEDD increased (6.2±11.3% vs. -3.1±6.1%; p<0.01), while for basketball players both RWT and LVEDD increased during the season. These findings are similar when only male soldiers and basketball players are compared, with significant differences in RWT (-10.0±14.3% vs. 21±25.3%; p=0.02), LVEDD (6.2±11.3% vs. -3.1 ±4.2%; p<0.01) and LVEF (-5.5±12.8% vs. 4.9±10.5; p<0.01).
Percentage differences in echocardiographic parameters between the study groups. GLS: global longitudinal strain; IVS: interventricular septum thickness; LVEDD: left ventricular end-diastolic diameter; LVEF: left ventricular ejection fraction; LVMI: left ventricular mass index; RWT: relative wall thickness.
This study demonstrated the occurrence of anthropometric and cardiovascular remodeling in both soldiers and basketball players. These adaptations had different characteristics in the two groups. In anthropometric terms, the soldiers had a greater increase in body weight, with gains in MM and reductions in FM. Echocardiographic assessment revealed different patterns of remodeling, with the soldiers developing predominantly eccentric and the basketball players developing mainly concentric adaptations.
The alterations in anthropometric data and vital signs following the military course or sports season were more significant in the soldiers’ group, even when a sub-analysis was performed (data not shown) comparing the soldiers with the Caucasian male athletes. There was a marked transformation in the body composition of the former group, with mean MM gains of 7.5% and mean FM reductions of around 30%. The differences in adaptation in the two groups may be related to the different characteristics of exercise in military training and in basketball, particularly the longer duration and greater intensity of exercise in military training, as well as specific features of the methodologies used. These differences likely explain the more marked adaptations in the soldiers. It has been shown that high-intensity interval training, in this case applied to the soldiers, achieves better results and greater adaptation.13 The mechanisms underlying this adaptation are still unclear, but this type of training is thought to enhance capacity for aerobic and anaerobic metabolism and to increase oxidative enzyme activity.14 Although there were no individuals with hypertension in either group, intense physical exercise led to reductions in the soldiers of around 4% and 9% in SBP and DBP, respectively. These results are in agreement with the literature.15
Cardiac remodeling occurred in both groups, but had different characteristics. In the soldiers, eccentric remodeling occurred with an increase in left chamber size and a decrease in RWT. At the end of the course, the proportion of soldiers with eccentric ventricular hypertrophy had doubled, from 5.9% to 11.8%.16 In the basketball players predominantly concentric remodeling was observed, with increases in LV wall thickness, particularly of the IVS, and RWT, and a slight decrease in LVEDD. One possible explanation for these different types of cardiac remodeling is the intensity of the exercise performed. Moderate- to high-intensity exercise is initially associated with concentric hypertrophy due to the stimulus of pressure overload.17 Vigorous- to near maximal- or maximal-intensity exercise leads to eccentric remodeling, due to volume overload from increased cardiac output, resulting from higher HR and increased ejection volumes, with only a moderate increase in BP.17,18 This moderate increase in BP seems to be associated with acetylcholine-induced endothelium-dependent vasorelaxation, which plateaus with moderate to vigorous levels of exercise.19 Thus, when the level of exercise increases from vigorous-intensity to near maximal- or maximal-intensity, there is a greater increase in cardiac output that is not accompanied by a proportional increase in BP, and this may lead to dilatation of the heart chambers that is disproportionate to the observed wall hypertrophy.
Despite the extent of the adaptations observed over the course or season, the changes were still within the upper limit of normal (no athlete with IVS >13 mm and only one with LVEDD >60 mm [61.4 mm]). There were also no statistically significant changes in parameters of diastolic function during the study. However, it should be noted that both soldiers and athletes already had above-normal values, as described in similar populations.20,21
Exercise-induced changes in functional parameters were also different in the two groups. In the soldiers, there was a decrease in resting LVEF, while in the basketball players this parameter remained similar to baseline values. The literature reports that elite athletes who are subject to intense and prolonged exertion may have slightly lower resting LVEF, with mean values of 50-55%, which increases as required when prompted by effort.22,23 In the soldiers, no individual had an LVEF <50% on the baseline or final echocardiogram; however, 12 soldiers (70% of the population) had an LVEF of 50-55% on the final exam.
Both the soldiers and the basketball players had GLS values within normal limits,7 with a trend toward reduction after the exercise program. This decrease was not significant when the two groups were analyzed separately. However, when they were compared, GLS decreased significantly. This behavior is consistent with that described in the literature,7 and may represent an exercise-induced physiological adaptation and another characteristic that distinguishes ‘athlete's heart’ from heart disease, particularly hypertrophic cardiomyopathy.24,25 However, the current scarcity of data in this area indicates a need for further studies designed to study the effect of physical exercise on this parameter.
LimitationsThe main limitation of this study is the small sample size for both special forces soldiers and athletes. The heterogeneity of the populations with regard to gender and race also limits the results, mainly because no female soldiers participated in the special forces course. Another limitation is the inability to objectively quantify unscheduled physical exercise performed by the soldiers during the course. These individuals are constantly involved in activities and assessments, in which the physical component is central, even when they are not performing conventional or scheduled exercise. Finally, although all of the participants strongly denied using stimulants, the study protocol did not enable this denial to be confirmed.
ConclusionIn this study, anthropometric and cardiac remodeling occurred in both special forces soldiers and competitive basketball players following a military course or sports season. This remodeling had different characteristics in the two groups, being predominantly eccentric in the soldiers and concentric in the basketball players. New echocardiographic techniques, particularly myocardial strain analysis, may reveal patterns that are compatible with physiological adaptation to exercise, and may help to differentiate between ‘athlete's heart’ and heart disease.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors thank the Centro de Tropas Comandos (Portuguese Army Commando Center) and Olivais FC basketball club.
Please cite this article as: Dinis P, Teixeira R, Dores H, Correia P, Lekedal H, Bergman M, et al. Remodelagem cardíaca induzida pelo exercício físico em atletas de nível competitivo e militares de forças especiais. Rev Port Cardiol. 2018;37:249–256.








 GLS) values; (B) transthoracic echocardiographic images of a basketball player after the sports season, with LV wall thickening near the upper normal limit and normal diastolic function parameters and
GLS) values; (B) transthoracic echocardiographic images of a basketball player after the sports season, with LV wall thickening near the upper normal limit and normal diastolic function parameters and 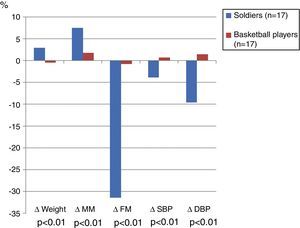 DBP: diastolic blood pressure; FM: fat mass; MM: muscle mass;
DBP: diastolic blood pressure; FM: fat mass; MM: muscle mass; 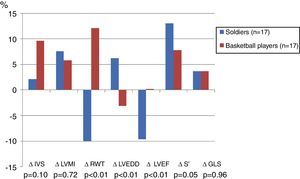 GLS: global longitudinal strain;
GLS: global longitudinal strain; 

