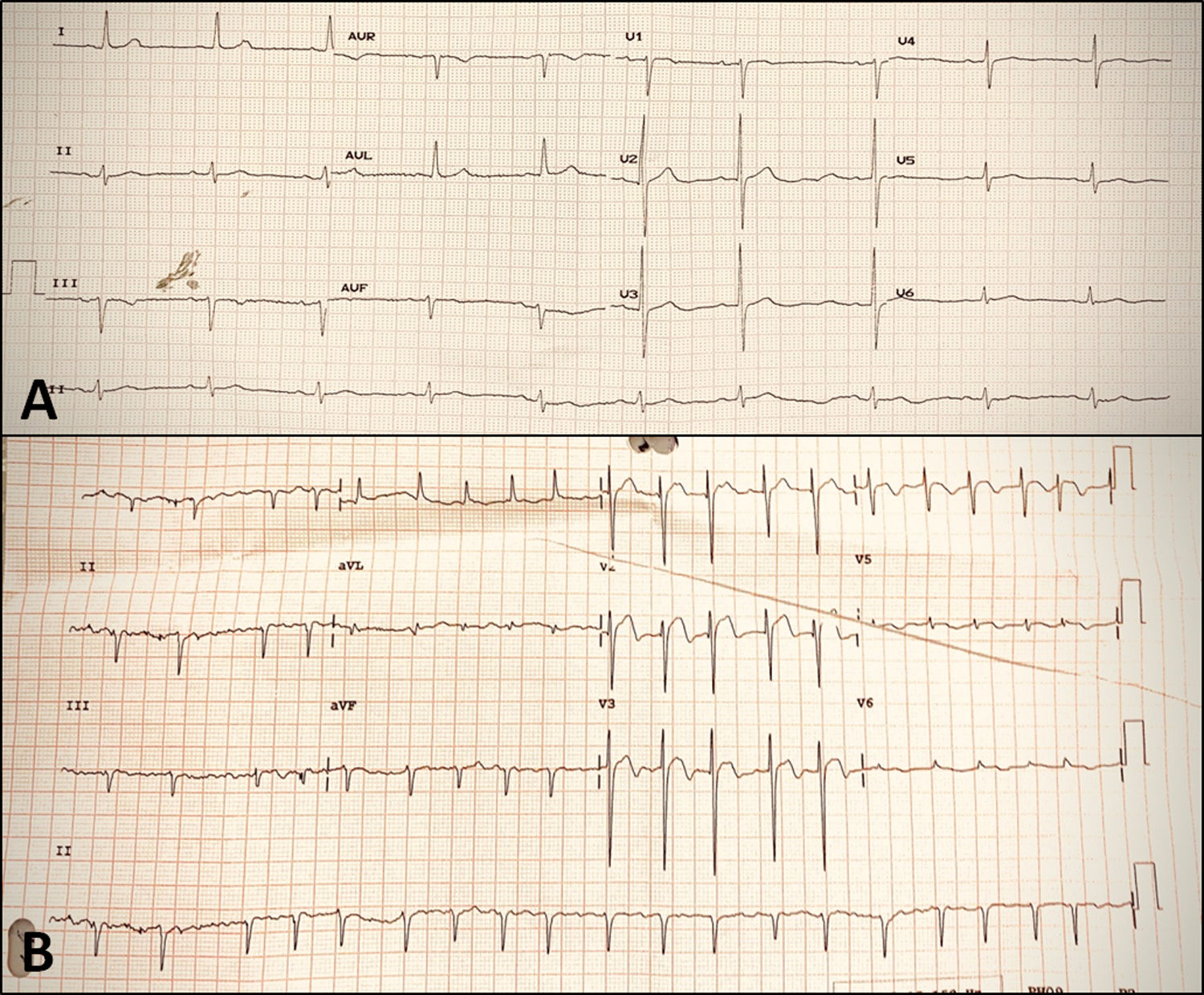
A 94-year-old female, with hypertension, paroxysmal atrial fibrillation, ischemic stroke and an echocardiogram without wall motion abnormalities performed the previous month, presented to the emergency department with a two-day history of dyspnea and dry cough without fever. The patient had had contact with a COVID-19 patient, PCR was positive for SARS-CoV-2 and the chest radiography documented bilateral basal pneumonia. The baseline electrocardiogram showed sinus rhythm without significant repolarization alterations (Figure 1A). The patient was hospitalized for treatment.
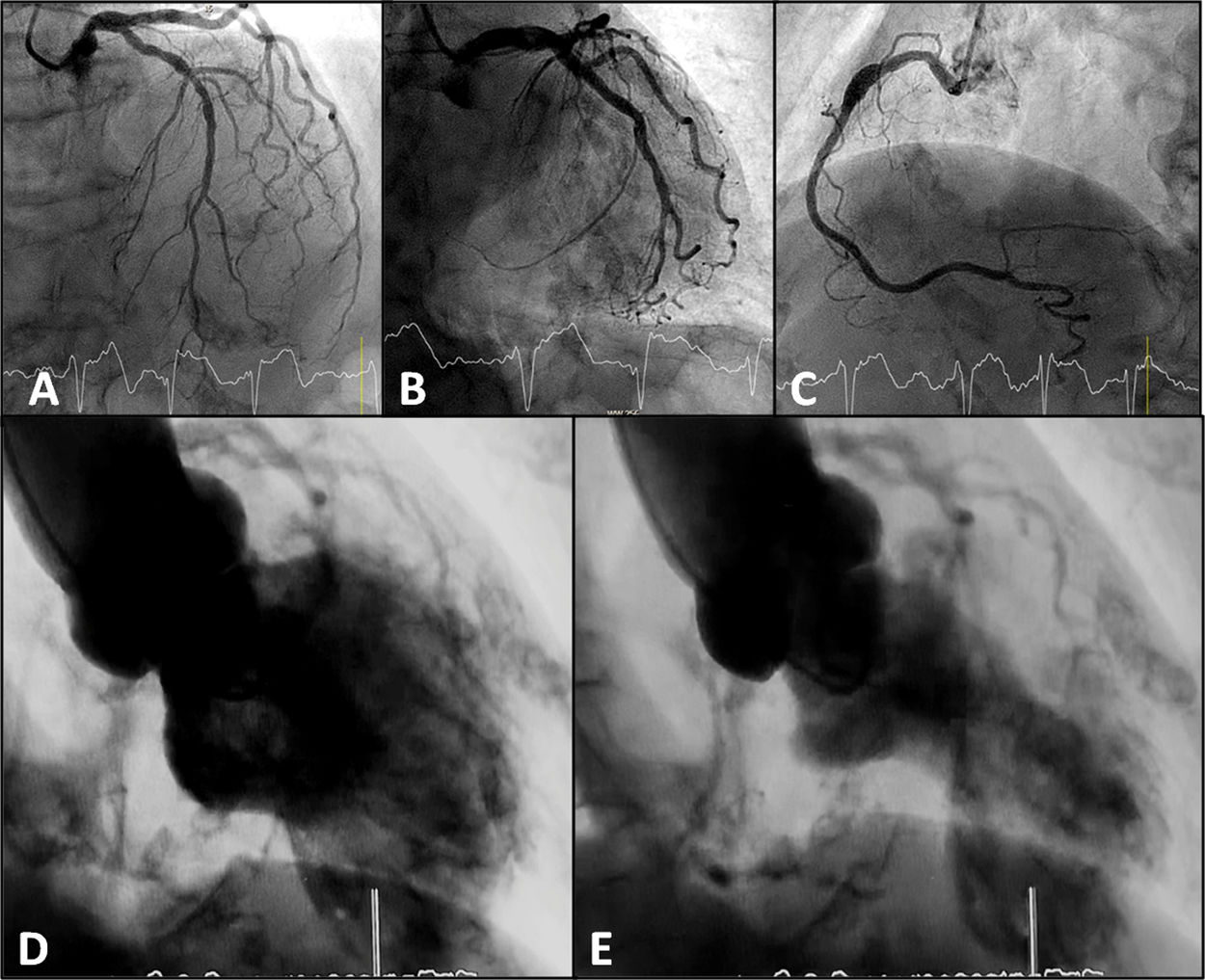
On the fifth day of hospitalization, the patient reported chest pain and the electrocardiogram showed atrial fibrillation with rapid ventricular response and ST-segment elevation in the anterolateral leads (Figure 1B). Emergent coronary angiography demonstrated absence of obstructive coronary lesions (Figure 2A-C; Videos 1-3) and ventriculography showed severe ventricular dysfunction with anterolateral, apical, and inferior dyskinesia and hypercontractility of the basal segments, compatible with Takotsubo syndrome (TTS) (Figure 2D and E; Video 4). At two-month follow-up, the patient remains asymptomatic and the echocardiogram demonstrated recovery of ventricular contractility.
Cardiac catheterization during primary percutaneous coronary intervention. (A-C) Coronary angiography with non-obstructive coronary artery disease; (D-E) ventriculography showing wall motion abnormalities in apical segments of the anterolateral and inferior walls, compatible with Takotsubo wall motion abnormality pattern.
The TTS consensus documents recommend coronary angiography and ventriculography to confirm the diagnosis. There are few reported cases of TTS triggered by COVID-19, with a non-negligible proportion diagnosed by echocardiography. The lack of invasive methods to confirm the diagnosis of TTS in COVID-19 patients could be related to the unavailability or the inherent risk of invasive tests. However, failure to perform coronary angiography and ventriculography can lead to false diagnoses. In this case, we show through invasive methods, following the recommended criteria, the development of TTS in a patient with COVID-19.
Conflicts of interestThe authors have no conflicts of interest to declare.