Coronary sinus (CS) atrial septal defect (ASD) is a very uncommon anomaly (accounting for <1% of all ASDs) that occurs as a result of a defect in the wall between the CS and the left atrium due to hypoplasia of the left atriovenous fold during embryonic development. CS dilatation of a different extent caused by an interatrial shunt is an important clue to the diagnosis, after other causes of the dilatation, such as elevated right atrial pressure, persistent left superior vena cava (PLSVC), and/or coronary artery fistula to the CS have been excluded.
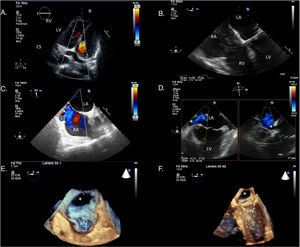
A 65-year-old woman with a previous history of paroxysmal atrial fibrillation was referred to our hospital for exertional dyspnea with marked limitation in her daily activity, even light activity, due to symptoms. Vital signs were normal and physical examination revealed mild ankle edema at the time of presentation. The ECG showed sinus rhythm with right bundle branch block as the only remarkable finding. Transthoracic echocardiography revealed biatrial and right ventricular enlargement with elevated systolic pulmonary pressure (60-65 mmHg) and preserved biventricular systolic function. Of note, CS dilatation was observed in 4-chamber view (Figure 1A). Agitated saline was injected through a peripheral left brachial vein during the Valsalva maneuver, but no right-to-left shunt or CS contrast enhancement was detected (Figure 1B). The injection was made through the left arm to exclude PLSVC. Transesophageal echocardiography showed CS drainage below the inferior vena cava in mid-esophageal bicaval view (Figure 1C) and in cross-sectional 2-chamber view a posteromedial left atrial wall defect communicating with the CS was detected (Figure 1D). Three-dimensional (3D) real-time acquisition confirmed a 29 mm×19 mm posteromedial left atrial wall defect communicating with the CS and draining into the right atrium, establishing the diagnosis of CS atrial septal defect (Figure 1E and F).
(A) Coronary sinus dilatation on transthoracic echocardiography (TTE), 4-chamber view; (B) agitated saline through a peripheral left brachial vein during the Valsalva maneuver; (C) mid-esophageal bicaval view with coronary sinus drainage below the inferior vena cava; (D) cross-sectional 2-chamber view showing a posteromedial left atrial wall defect communicating with the coronary sinus; (E and F) three-dimensional real-time TEE with the mitral valve (MV) as reference point and the left atrial wall defect marked with an asterisk.
3D real-time transesophageal echocardiography is a valuable tool for detailing the type of roof defect and for identifying abnormal positions of the CS ostium. The combination of both imaging modalities (transthoracic and 3D real-time transesophageal echocardiography) may improve the diagnosis of this rare congenital heart defect.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.