Patients with obstructive coronary artery disease and severe aortic stenosis have traditionally been managed with open heart surgery. In the era of transcatheter aortic valve replacement (TAVR) and high-risk coronary interventions many of those patients who were previously considered “terminal” can now be successfully managed with percutaneous coronary intervention (PCI) and TAVR. Although simple PCI can be safely combined with TAVR in the same procedure, high-risk coronary interventions often need to be performed separately. We report the first case of combined rotational atherectomy with balloon aortic valvuloplasty as a bridge to TAVR in a frail patient with complex coronary artery disease and critical aortic stenosis.
O grupo de doentes com doença coronária obstrutiva e estenose aórtica grave foi tratado, conforme é habitual, com cirurgia de coração aberto. Na era de substituição valvular aórtica percutânea (TAVR) e das intervenções coronárias de alto risco, muitos daqueles doentes que foram previamente considerados «terminais», podem agora ser tratados com sucesso com intervenção coronária percutânea (ICP) e com TAVR. Embora a simples ICP possa ser prudentemente combinada com a TAVR no mesmo procedimento, as intervenções coronárias de alto risco necessitam muitas vezes de ser efetuadas em separado. Apresentamos o primeiro caso clínico de aterectomia rotacional combinada com valvuloplastia aórtica com balão como ponte para TAVR numa doente frágil com doença coronária complexa e estenose aórtica crítica.
The combination of symptomatic obstructive coronary artery disease (CAD) and severe aortic stenosis (AS) accounts for 25–50% of patients with severe AS and carries important morbidity and mortality.1–3 The standard of care has traditionally been surgical aortic valve replacement (SAVR) with coronary artery bypass grafting (CABG). Although isolated SAVR generally carries a low surgical risk, the additional need for CABG significantly raises surgical mortality, especially in the frail and elderly population.4–6 Furthermore, incomplete coronary artery revascularization in patients with SAVR is known to increase postoperative mortality.7
In the era of transcatheter aortic valve replacement (TAVR) many patients with obstructive CAD and AS who are not candidates for surgery are referred for transcatheter management.
We present a case of complex obstructive CAD with critical AS, treated with combined rotational atherectomy and aortic valvuloplasty as a bridge to TAVR.
Case reportAn 84-year-old female with severe symptomatic aortic stenosis was referred to our multidisciplinary team for possible SAVR or TAVR. For the last six months she had experienced progressive angina (Canadian Cardiovascular Society class III) and dyspnea on exertion (New York Heart Association class III) with a recent episode of syncope which resulted in a forehead laceration and ecchymosis. The patient was wheelchair-bound for more than two months due to the presence of activity-limiting symptoms.
Her transthoracic echocardiogram revealed a non-dilated left ventricle with preserved ejection fraction of 60% and moderate concentric hypertrophy. The aortic valve was trileaflet, heavily calcified with a peak transaortic velocity of 5.2 m/s, a mean pressure gradient (PG) of 55 mmHg, a calculated aortic valve area (AVA) of 0.37 cm2, an AVA index of 0.26 cm2/m2 and absence of aortic insufficiency. The right heart chambers were non-dilated, with mild pulmonary hypertension of 45 mmHg, and the mitral valve showed normal morphology and function.
A previous nuclear stress test performed by the primary care provider before the diagnosis of aortic stenosis revealed a large area of inferior wall ischemia. Consequently, we scheduled an invasive coronary angiogram with left and right heart catheterization, which showed a heavily calcified ostial right coronary artery obstructive lesion of 99% (Figure 1) combined with critical aortic stenosis (mean transaortic PG of 44 mmHg and an AVA of 0.3 cm2).
Taking into consideration her overall functional condition, comorbidities and a Society of Thoracic Surgeons (STS) score of 12%, our multidisciplinary team concluded that a transcatheter approach was preferable to open heart surgery. We elected to perform a high-risk percutaneous intervention of the RCA with BAV as a bridge to a staged TAVR. Due to the RCA complexity, requiring an important volume of contrast for PCI, we decided to proceed for a staged PCI of the RCA combined with balloon aortic valvuloplasty (BAV), followed by TAVR after recovery. We felt that this approach would limit the amount of contrast used and would allow conscious sedation and the use of smaller sheaths. We anticipated that the first stage would temporarily improve the patient's angina and functional class for a safer second-stage ad-hoc TAVR procedure. At the same time, in the event of hemodynamic instability during rotational atherectomy or BAV, bail-out emergent TAVR or open surgery could be performed in our hybrid lab.
A 7 French (F) sheath was placed in the left common femoral artery (CFA), after preclosure with two Perclose ProGlide suture-mediated closure systems (Abbott Vascular, Abbott Park, IL) and a 6F sheath in the right femoral vein. A 7F JR4 guiding catheter with side holes was placed in the ostium of the RCA and a 6F temporary pacemaker lead was positioned and secured in the right ventricle.
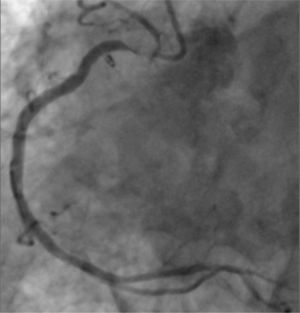
The RCA lesion was crossed with a RotaWire Floppy Guide Wire (Boston Scientific, Natick, MA), which was advanced to the distal RCA. Rotational atherectomy was performed with several passes of a 1.5 mm burr. During rotational atherectomy we aimed to maintain the patient's heart rate 15–20 bpm above resting heart rate to prevent any potential bradycardia and subsequent hypotension. A 3.0 mm×12 mm Resolute drug-eluting stent (DES) (Medtronic, Minneapolis, USA) was deployed in the ostium of the RCA at 18 atm and post-dilated with a 3.5 mm×12 mm non-compliant balloon, with an excellent angiographic result (Figure 2).
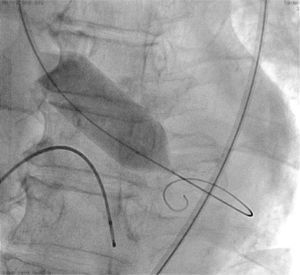
After completion of the coronary intervention, the 7F arterial sheath was upsized to an 11F sheath. The aortic valve was crossed with an AL-1 diagnostic catheter and a soft straight 0.035″ guide wire which was then exchanged for an Amplatz Super Stiff wire (St. Jude, St. Paul, MN). BAV was performed with a 20 mm Loma Vista balloon (Loma Vista Medical Inc.) under rapid pacing (Figure 3).
Postvalvuloplasty hemodynamics revealed a residual mean gradient of 23 mmHg and an estimated aortic valve area of 0.56 cm2. The procedure was then terminated with no immediate or late complications.
The patient remained asymptomatic until a successful TAVR procedure four weeks later.
DiscussionPatients with obstructive coronary artery disease and severe aortic stenosis have traditionally been managed with open heart surgery. In the era of TAVR and high-risk coronary interventions many of those patients who were previously considered “terminal” can now be successfully managed with PCI and TAVR. The medical literature on the optimal transcatheter management of such cases is scant and the appropriate approach and strategy are unclear.8
In the absence of randomized control trials (RCTs), as the only RCT involving TAVR (the PARTNER trial) excluded patients with obstructive CAD, data from registries and case series clearly show significant increased long-term mortality in patients with combined CAD and AS.1
Although the role of BAV as a definitive treatment is now limited, it remains an acceptable bridge to SAVR or TAVR in patients who are not immediately suitable for permanent treatment.9
The optimal timing of each procedure also remains unclear.9,10 Pedersen et al. suggested that BAV with PCI may be as safe as BAV alone in selected patients.10
In a large retrospective cohort study, Goel et al. showed that PCI in patients with severe symptomatic AS does not increase the risk of short-term mortality.8 However, in patients with ejection fraction <30% or STS score >10%, increased 30-day mortality after PCI was seen.
In a smaller case series, Salhab et al. demonstrated the feasibility and safety of PCI and TAVR in the same procedure.11 In the real world, due to fluoroscopy time and contrast volume limitations, such an approach is reserved for patients with simple PCIs and without anticipated important hemodynamic compromise.
The safety of rotational atherectomy in patients with severe aortic stenosis has not been well established. Combined rotational atherectomy and BAV have been previously reported as separate staged procedures or in the same procedure with hemodynamic support devices.12,13
We present the first case report of combined rotational atherectomy with BAV as a bridge to TAVR in a frail patient with symptomatic combined obstructive CAD and critical AS who was deemed inoperable. Although we did not use hemodynamic support devices, we elected for temporary pacing at higher heart rates during rotational atherectomy to prevent atherectomy-induced bradycardia and hypotension.
ConclusionThe optimal management of inoperable patients with obstructive CAD and severe AS remains unclear. In cases with high-risk coronary lesions, PCI with BAV may represent a reasonable first procedure as a bridge to TAVR. Our case report, the first of its kind, of combined rotational atherectomy and BAV without hemodynamic support shows that high-risk coronary interventions are feasible in patients with critical AS with careful planning. Larger studies are needed to define the best transcatheter approach and strategies.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.