What is the clinical impact of oxygen therapy for acute myocardial infarction?
Description of reviewThis is a systematic review of randomized controlled trials (RCTs) on routine use of inhaled oxygen in patients with acute myocardial infarction (AMI) (ST-segment elevation myocardial infarction [STEMI] or non-STEMI) within the first 24 hours after the onset of symptoms. The primary outcome was overall mortality; the secondary outcome was opiate use as a surrogate outcome for pain.
ResultsThe Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, CINAHL and Web of Science were searched and the eligibility of the results was assessed. Four RCTs were included for the qualitative and quantitative analysis, involving 430 patients and 17 deaths. Studies in which hyperbaric or aqueous oxygen, oxygen associated with hemoglobin, or oxygen combined with nitric oxide were excluded.
In the selected studies, oxygen was administered at 4–6 l/min by facial mask or nasal cannula. Oxygen therapy was compared with no oxygen administration or its use only in cases of hypoxemia.
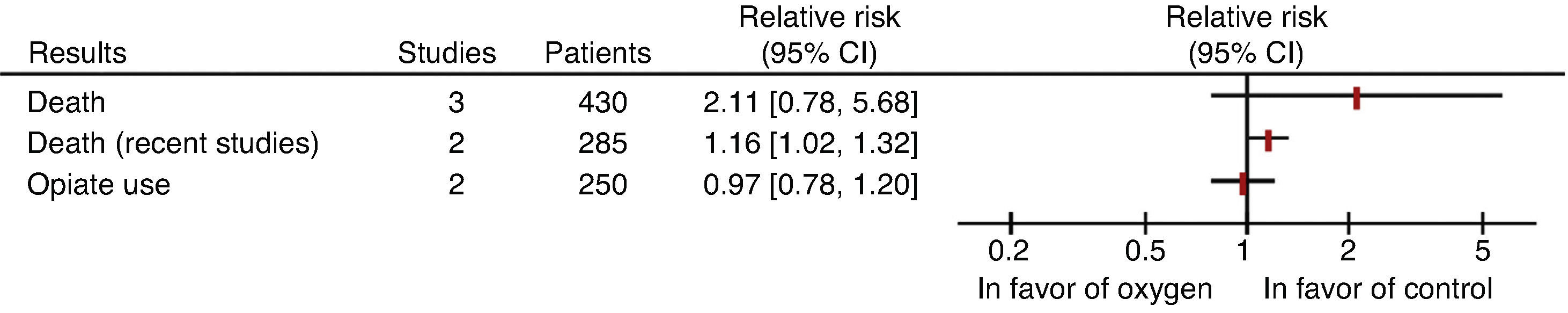
The relative risks of death and opiate use were not significantly different between groups (Figure 1), and a significant increase (16%) in risk of death was observed in the oxygen therapy arm in the two most recent RCTs. The small number of deaths does not exclude that this may be due to chance.
Main results of the systematic review by Cabello et al.1 CI: confidence interval.
There is no conclusive evidence from RCTs to support the routine use of inhaled oxygen in people with AMI.
CommentThis systematic review1 highlights the scarcity of clinical trials assessing oxygen therapy in patients with AMI, which is a common practice in the treatment of these patients. The best available evidence suggests that there is no benefit in either mortality or pain relief (assessed using opiate use as a proxy).
Oxygen therapy is common practice in patients with AMI and according to cross-sectional studies many health professionals (>50%) consider that oxygen reduces mortality, and around 80% routinely administer oxygen in cases of AMI.2,3
This attitude is strengthened by the mechanistic belief that increased oxygen supply reduces ischemia and hence pain and mortality. However, the results of the meta-analysis suggest that routine use of this intervention tends to increase mortality, which may be explained by oxygen's vasoconstrictor properties,4 leading to increased vascular resistance and reducing coronary flow.5
Nevertheless, the results of this review should be considered in the light of the limitations of the individual studies, the low overall methodological quality, with a high risk of attrition bias due to loss of follow-up data after randomization, and of bias due to selective outcome reporting. Another limitation is related to changes in the way that acute coronary syndromes are treated; nowadays patients routinely receive therapies that have a significant impact on prognosis, including dual antiplatelet therapy, beta-blockers, angiotensin-converting enzyme inhibitors, statins, and coronary revascularization. Sensitivity analysis excluding the older studies to assess the effect of oxygen therapy on mortality in contemporary practice supports the conclusion that routine oxygen therapy has no clinical benefit in these patients.
It should also be considered that most of the studies in the review included different pathophysiological entities with different treatments (STEMI and non-STEMI), and so the real impact of oxygen therapy in these different contexts is not known.
In contrast to the results of this review, another Cochrane review6 of six clinical trials with 665 patients with acute coronary syndrome estimated that hyperbaric oxygen therapy reduced the relative risk (RR) of death by 42% (RR 0.58, 95% CI 0.36–0.92). This result prompts the question as to whether the negative findings of the review under discussion are due to its low statistical power and/or methodological weaknesses.7
The current guidelines of the European Society of Cardiology only recommend oxygen therapy in cases of hypoxemia.8,9
The clinical question posed here clearly needs to be answered definitely by future pragmatic clinical trials with an appropriate design and size.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Caldeira D, Vaz-Carneiro A, Costa J. Cochrane Corner – qual é o impacto clínico da administração sistemática de oxigénio em doentes com enfarte agudo do miocárdio? Avaliação da revisão sistemática: Cabello JB, Burls A, Emparanza JI, Bayliss S, Quinn T. Oxygen therapy for acute myocardial infarction. Cochrane Database Syst Rev. 2014 Aug 21;8:CD007160. Rev Port Cardiol. 2014;33:641–643.