This study aims to characterize patients hospitalized for acute heart failure (HF) in an internal medicine department and their one-year mortality and rate of rehospitalization for decompensated HF.
MethodsThis retrospective observational study enrolled all patients discharged in 2012 after hospitalization for acute HF. Discharge summaries, clinical records and telephone interviews were analysed. The data reports to the year before implementation of a heart failure clinic.
ResultsFour hundred and twenty-nine patients were enrolled, with a mean age of 79 years, 62.5% female. The most prevalent comorbidity and etiology was hypertension (86.7%) and the most frequent decompensation trigger was infection. HF with preserved ejection fraction (HFpEF) was present in 70.5%. In-hospital mortality was 7.9%. At discharge more than half of the patients were prescribed beta-blockers (52.8%) and angiotensin-converting enzyme inhibitors (52%). Women presented a significantly higher proportion of HFpEF than men (75.3% vs. 62.7%, p=0.01). Patients with diabetes and those with ischemic etiology had significantly higher proportions of HF with reduced ejection fraction (HFrEF) (34.8% vs. 24.3% in non-diabetic patients, p=0.027, and 56.2% vs. 15.6% for other etiologies, p<0.001). The HFrEF group were more frequently discharged under beta-blockers and spironolactone (75.2% vs. 46.4% in the HFpEF group, p<0.001 and 31.2% vs. 12.6% in the HFpEF group, p<0.001, respectively). Mortality was 34.3% and rehospitalization for HF was 30.5% in one-year follow-up.
ConclusionsThe population characterized is an elderly one, mainly female and with HFpEF. Nearly a third of patients died and/or were rehospitalized in the year following discharge.
Caracterizar os doentes hospitalizados por Insuficiência Cardíaca (IC) aguda num Serviço de Medicina Interna, a mortalidade e rehospitalização por IC no primeiro ano.
MétodosEstudo retrospetivo observacional incluindo todos os doentes com alta em 2012 de hospitalização por IC aguda, com base em Notas de Alta, registos clínicos e entrevistas telefónicas. Reporta-se ao ano prévio à implementação de uma clínica de IC.
ResultadosIdentificaram-se 429 doentes, com idade média de 79 anos; 62,5% eram mulheres. A comorbilidade e etiologia mais prevalente foi a hipertensão arterial (86,7%) e o fator precipitante mais frequente da descompensação foi a infeção. Verificou-se Fração de Ejeção Preservada (FEp) em 70,5% dos doentes. A mortalidade intra-hospitalar foi 7,9%. À alta, a maioria dos doentes tinha prescrição de betabloqueadores (BB) (52,8%) e inibidores de enzima de conversão da angiotensina (52%). As mulheres apresentaram mais frequentemente FEp do que os homens (75,3% versus 62,7%, p=0,01). Os doentes diabéticos e os com etiologia isquémica apresentaram mais frequentemente Fração de Ejeção Reduzida (FEr) (34,8% versus 24,3% em não diabéticos, p=0,027 e 56,2% versus 15,6% com outras etiologias, p<0,001, respetivamente). No grupo com FEr, os BB e a espironolactona foram mais prescritos à alta (75,2% versus 46,4% no grupo com FEp, p<0,001 e 31,2% versus 12,6% no grupo com FEp, p<0,001, respetivamente). No primeiro ano, a taxa de mortalidade foi 34,3% e de rehospitalização por IC 30,5%.
ConclusõesA população estudada é idosa, predominantemente feminina e apresenta IC com FEp. Um terço morreu e/ou foi reinternada no ano seguinte.
angiotensin-converting enzyme
atrial fibrillation
angiotensin receptor blocker
ejection fraction
heart failure
heart failure with preserved ejection fraction
heart failure with reduced ejection fraction
International Classification of Diseases, 9th Revision
non-invasive ventilation
N-terminal-pro-B type natriuretic peptide
Heart failure (HF) is a major global burden in terms of patients’ quality and duration of life and of health expenditure.1–4 Approximately 1-2% of the adult population in developed countries has HF, the prevalence rising to ≥10% among those 70 years of age or older.1,5,6 In Portugal, the overall prevalence of chronic HF was 4.36% in a community-based epidemiological survey carried out in 1998, rising sharply with age; this was slightly higher than that of other European countries.7
Across the globe, 17-45% of patients hospitalized with HF die within a year of hospitalization3,4,8 and a quarter are rehospitalized within one month and up to two-thirds within a year.1,8–10 HF is the most common reason for hospitalization in people over 65 years of age in economically developed regions.6,9,11–13
According to national registries of the Portuguese Directorate-General of Health, in 2014 18 588 patients were hospitalized for HF and the in-hospital mortality rate was 12.5%.14
The increasing incidence of acute HF and associated morbidity and mortality mean there is an urgent need to better understand this patient population.15 Despite the high prevalence of acute HF, few studies have been conducted specifically in the hospitalized HF population, and data on clinical characteristics and outcomes for these patients are lacking, especially in Portugal. Observational studies provide useful information about real-world patients and routine clinical practice.2 Interest in this type of research has been growing in recent decades, for various reasons.4
According to the latest guidelines on heart failure, the standard-of-care for HF patients recently hospitalized for acute de novo or chronic decompensated HF should include enrollment in a multidisciplinary care management program,5,16 also known as a heart failure clinic.17
The present study covers the year before the implementation of an HF clinic, using a multidisciplinary approach to HF patients, in a Portuguese tertiary university hospital. The study was designed to improve knowledge of the characteristics of patients hospitalized and treated for HF in an internal medicine department and to present one-year follow-up outcomes, reporting in-hospital and one-year mortality and rehospitalization for HF, which will help to evaluate the impact of our HF clinic on those outcomes.
MethodsStudy design and clinical settingThis was a single-center retrospective observational study. All patients hospitalized in the internal medicine department of a tertiary university hospital and discharged between January 1 and December 31, 2012 were considered for enrollment. The study population was selected using the International Classification of Diseases, 9th Revision (ICD-9) codes, as listed in the discharge summary. All discharge summaries reporting one of the ICD-9 HF codes (428, 428.0, 428.1, 428.2, 428.3, 428.4, 428.9, 402.01, 402.11, 402.91 or 398.91) in the first three codes were reviewed. Based on review of the discharge summary, patients were selected if they had been hospitalized for acute, de novo or chronic decompensated HF as stated in their medical record, and were aged 18 years or older. HF was diagnosed according to European Society of Cardiology guidelines.5 All patients without an echocardiogram had relevant cardiac disease documented in their clinical record and NT-proBNP values higher than 1000 pg/ml.
For the purposes of the study, the first hospitalization for acute HF in the study period was considered the index hospitalization.
Data collectionData were collected based on discharge summaries, medical records and telephone interviews.
The following data were collected from the discharge summary: gender, age, risk factors for HF, comorbidities, functional status, HF etiology, decompensation trigger and treatment. HF comorbidities considered for analysis were hypertension, diabetes, cerebrovascular disease, peripheral arterial disease, atrial fibrillation (AF), active cancer, chronic lung disease, sleep apnea and/or hypoventilation syndrome, and dementia.
Other clinical records were reviewed for biometric, laboratory, echocardiographic, follow-up and rehospitalization data. The etiology of cardiac disease was established through clinical data and echocardiography. Only rehospitalizations at the study center were considered.
Mortality data were obtained through clinical records and telephone interviews.
OutcomesThe main outcomes were the characteristics of the study population, namely age, gender, comorbidities, HF risk factors and etiology, HF decompensation trigger, left ventricular ejection fraction (EF), in-hospital mortality, discharge treatments, rehospitalization for decompensated HF and death in the year following discharge from the index hospitalization.
Study oversightThe two lead authors prepared the manuscript, and all authors reviewed it. All the authors vouch for the accuracy and completeness of the data and analysis.
Statistical analysisCategorical variables are presented as percentages, while continuous variables are presented as means and standard deviation (SD) plus median and interquartile range (IQR). Proportions were compared using the chi-square test for categorical variables. The statistical analysis was performed using SPSS for Windows, version 22.
ResultsPatients and comorbiditiesIn the study period 429 patients were identified and analyzed, as depicted in Figure 1. The characteristics of the study group are reported in Table 1. Mean age was 79 years and the majority of patients were female (62.5%). The most prevalent comorbidity was hypertension, followed by AF and diabetes.
Characteristics of the study population.
| n | ||
|---|---|---|
| Age (years), mean ± SD; median (IQR) | 79±10; 81 (11) | 429 |
| Female, % | 62.5 | 429 |
| Ischemic etiology, % | 34.6 | 402 |
| Admission SBP (mmHg), mean ± SD; median (IQR) | 139.5±29.2; 136 (36) | 420 |
| Ejection fraction >40%, % | 70.5 | 400 |
| Hypertension, % | 86.7 | 429 |
| Diabetes, % | 47.8 | 429 |
| AF, % | 51.7 | 429 |
| Cerebrovascular disease, % | 19.1 | 429 |
| Peripheral arterial disease, % | 11.7 | 429 |
| Chronic pulmonary disease, % | 28 | 429 |
| Active cancer, % | 6.8 | 429 |
| Sleep apnea/hypoventilation syndrome, % | 19.3 | 429 |
| Dementia, % | 24.7 | 429 |
| >3 comorbidities, % | 31.9 | 429 |
| Physically active, % | 77.6 | 429 |
| HF decompensation trigger | 429 | |
| Infection, % | 39.4 | |
| Non-adherence to treatment, % | 17.5 | |
| Rhythm disturbances, % | 16.1 | |
| Anemia, % | 4.9 | |
| Plasma creatinine >1.5 (mg/dl) %) | 30.8 | 428 |
| Admission plasma creatinine (mg/dl), mean ± SD; median (IQR) | 1.3±0.6; 1.2 (0.78) | 428 |
| Admission sodium (mmol/l), mean ± SD; median (IQR) | 136.4±5.7; 137 (6) | 428 |
| Hemoglobin (g/dl), mean ± SD; median (IQR) | 12±2.1; 12 (2.8) | 429 |
| First NT-proBNP (pg/ml) | 6698±10848; 2697 (6105) | 366 |
AF: atrial fibrillation; IQR: interquartile range; NT-proBNP: N-terminal-pro-B type natriuretic peptide; SBP: systolic blood pressure; SD: standard deviation.
On average, each patient had three comorbidities. A third of patients had more than three comorbidities.
Regarding functional ability, 96 patients (22.4%) had severe disability, being completely dependent on a caregiver for their daily needs.
Heart failureIschemic etiology of HF was recorded in 139 patients (34.6%) and valve disease in more than 74 (18.4%), of which severe aortic stenosis was the most common, found in 27 patients (6.7%) (data not shown). An echocardiogram was available in 400 patients, most of them with HF with preserved ejection fraction (HFpEF) (70.5%), defined as EF >40%, and only 36 patients (9%) had EF ≤25%.
The most frequent HF decompensation trigger was infection, followed by non-adherence to treatment and rhythm disturbances (Table 1). A trigger was not found in only two cases.
Non-invasive ventilationDuring hospital stay, 80 patients (18.6%) were treated with non-invasive ventilation (NIV), 51% of whom were not diagnosed with sleep apnea/hypoventilation syndrome.
Discharge medicationAt discharge, 394 patients were alive and prescribed appropriate cardiovascular medications, as reported in Table 2. About half of the patients discharged were prescribed a beta-blocker and an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin receptor blocker (ARB). Beta-blockers were prescribed significantly more frequently for patients with HF with reduced ejection fraction (HFrEF) but ACE inhibitors/ARBs were not.
Medications prescribed at discharge for the 394 patients discharged alive.
| Patients Drug | All | HFrEFa | HFpEFa | p |
|---|---|---|---|---|
| Beta-blocker | 52.8 | 75.2 | 46.4 | <0.001 |
| ACE inhibitor/ARB | 52.0 | 58.7 | 51.3 | 0.237 |
| Spironolactone | 17.3 | 31.2 | 12.6 | <0.001 |
| Anticoagulant | 29.9 |
ACE: angiotensin-converting enzyme; ARB: angiotensin receptor blocker; HFpEF: heart failure with preserved ejection fraction; HFrEF: heart failure with reduced ejection fraction.
Values refer to percentage of patients discharged in each group.
Oral anticoagulants were prescribed for 118 (29.9%) patients, mainly to the 201 patients with a history of AF (83.1%), of whom 48.8% had anticoagulants prescribed at discharge, while only 10.4% of those without AF received anticoagulation (p<0.001). This represents 20 patients anticoagulated for reasons other than AF, mainly arterial peripheral disease, venous thromboembolism, previous ischemic stroke or mechanical prosthetic cardiac valves; only two had a history of intracardiac thrombus (data not shown). The small number of patients prevents further statistical analysis.
Relation between ejection fraction and other clinical characteristicsThe relations between EF and characteristics including age, gender, HF etiology, comorbidities, plasma creatinine at admission and HF drug therapy prescribed at discharge are presented in Table 3. Women presented a significantly higher proportion of HFpEF than men.
Relation between ejection fraction and other characteristics.
| HFrEF | HFpEF | p | |
|---|---|---|---|
| Age | 0.439 | ||
| <80 years | 31.7 | 68.3 | |
| ≥80 years | 27.6 | 72.4 | |
| Gender | 0.010 | ||
| Female | 24.7 | 75.3 | |
| Male | 37.3 | 62.7 | |
| Ischemic etiology | <0.001 | ||
| Yes | 56.2 | 43.8 | |
| No | 15.6 | 84.4 | |
| Hypertension | 0.216 | ||
| Yes | 28.3 | 71.7 | |
| No | 38.3 | 61.7 | |
| Diabetes | 0.027 | ||
| Yes | 34.8 | 65.2 | |
| No | 24.3 | 75.7 | |
| AF | 0.704 | ||
| Yes | 30.6 | 69.4 | |
| No | 28.4 | 71.6 | |
| Cerebrovascular disease | 0.637 | ||
| Yes | 32.4 | 67.6 | |
| No | 28.8 | 71.2 | |
| PAD | 0.176 | ||
| Yes | 38.8 | 61.2 | |
| No | 28.2 | 71.8 | |
| Chronic pulmonary disease | 0.189 | ||
| Yes | 24.3 | 75.7 | |
| No | 31.6 | 68.4 | |
| Active cancer | 0.522 | ||
| Yes | 22.2 | 77.8 | |
| No | 30.0 | 70.0 | |
| Sleep apnea/hypoventilation syndrome | 0.095 | ||
| Yes | 21.3 | 78.8 | |
| No | 31.6 | 68.4 | |
| Dementia | 0.782 | ||
| Yes | 31.2 | 68.8 | |
| No | 29.0 | 71.0 | |
| Plasma creatinine>1.5 mg/dl | 1.000 | ||
| Yes | 29.6 | 70.4 | |
| No | 29.6 | 70.4 | |
AF: atrial fibrillation; PAD: peripheral arterial disease.
Data on 400 patients with ejection fraction estimated by echocardiography. Values refer to percentage of patients in each group.
Patients with diabetes and those with ischemic etiology had significantly higher proportions of HFrEF. The HFrEF group were more frequently prescribed beta-blockers and spironolactone at discharge (Table 2). Age, other comorbidities and plasma creatinine at admission were found to have no statistical relation with EF.
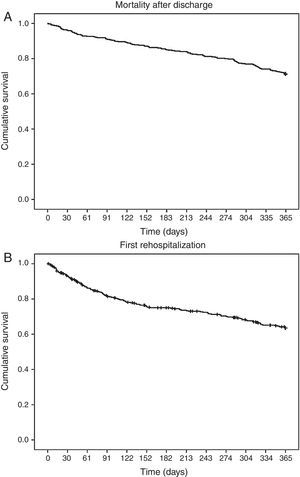
Follow-up outcomesIn-hospital mortality was 7.9%. Mortality in one-year follow-up was 34.3% (Figure 2A). One patient was lost to follow-up after discharge. The cause of death was established in 136 patients (92.5% of deaths) and a cardiovascular cause was found in 42.9% (data not shown).
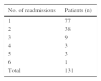
Rehospitalization at least once for HF occurred in 30.5% of patients during the first year of follow-up, within a median of 86 days (IQR 176) after discharge (Figure 2B). The number of rehospitalizations per patient ranged between one and six (Table 4).
During the first year of follow-up after discharge, 62% of patients had an outpatient appointment with a cardiologist or an internist in our hospital. It was not determined which patients were followed previously by one of these specialties or whether the appointment was scheduled prior to the HF hospitalization. The median time between discharge and appointment was 63 days (IQR 64.5).
Regarding potential admission to our HF clinic, 73% of patients were considered candidates. Referral to the clinic is considered for all patients hospitalized for acute HF. Exclusion criteria are total dependence on caregivers for basic daily needs and inability to communicate.
DiscussionThe main results of this study consist of the clinical findings of a large population hospitalized for HF in the internal medicine department of a tertiary university hospital. In Portuguese hospitals, many HF patients are treated by internists, even in hospitals where there is a cardiology department,18,19 so this is a real-world survey, enrolling all patients discharged following hospitalization due to acute or chronic decompensated HF during a one-year period.
Our patients are older, more frequently female and more often with HFpEF than HF patients in other series, who tend to be mainly hospitalized in cardiology departments.2,4 The mean age is similar to that reported in a recent French single-day survey in 170 hospitals of all patients hospitalized for acute HF,13 but 10 years older than in a recent Portuguese study enrolling patients hospitalized for acute HF only in the cardiology department of the other tertiary university hospital in the city where our study took place. In that study 73.2% of patients had HFrEF, which reflects considerable differences between the two study populations and is evidence of how observational studies provide valuable information about acute HF managed in different clinical scenarios.20,21 Our data on gender are in agreement with other reports showing that elderly patients hospitalized with HF are mainly women22 and that patients with HFpEF are older and more often female than those with HFrEF.1,5,6,8,13 HF patients managed by internists are more likely to have the characteristics of those managed by general practitioners. In the UK, the mean age of HF patients in general practice is 77 years, similar to that of our population. The HF patient seen in general practice is generally 15 years older, more often female, more likely to have a history of hypertension and less likely to have had myocardial infarction than the HF patient seen by a cardiologist.1,6 It has been shown that in Portugal chronic HFpEF mainly affects older women7 and that patients aged over 75 hospitalized for acute HF in an internal medicine department mainly have HFpEF.19
The average of three comorbidities per patient shows the complexity of this population and is in agreement with data on older people with HF in the USA.16 Of note, the prevalences of the two commonest comorbidities, hypertension and diabetes, in our study were similar to that report; this is not the case for AF, which was twice as common in the present study.16 Patients with more than three comorbidities have a higher risk of death and HF hospitalization, as shown by van Deursen et al.,23 although in their study only non-cardiovascular comorbidities were analyzed. Another study, on incident HF, reported that patients with HFpEF were more likely to have both cardiac and non-cardiac comorbidities.24
AF and a history of hypertension were more prevalent in this study population than in others in which HFrEF was more prevalent than HFpEF and patients were enrolled in cardiology wards.2,4 This is consistent with the literature on HFpEF populations and with data on Portuguese HF patients.4,19,25
Hypertension was the main etiology for HF, according to its prevalence in this population, but the retrospective nature of the study and the non-invasive diagnostic methods used for determining HF etiology prevent further analysis.
An ischemic etiology was less prevalent (34.6%) than reported by the above-cited European observational trials, which included mostly HFrEF patients (42%-50.7%), as expected.1,3,4,13 It is known that patients with HFpEF are less likely to have coronary heart disease and more likely to have hypertension and AF than those with HFrEF.5,6 We confirmed that ischemic HF patients more often had HFrEF.
The patient characteristics in this study were similar to those reported by a Spanish heart failure unit in a recent paper from the internal medicine department of a tertiary referral hospital, which describes an elderly population with a mean age of 80.3 years, of whom 54.8% were female, 72.2% had HFpEF (≥50% according to the criteria of this study) and the main etiologies were ischemic and hypertensive in the HFpEF group and ischemic in the HFrEF group.26
Infection was the most frequent trigger of HF decompensation in our study, as has been found in other Portuguese and European surveys.7,13,25
In addition to the significant correlation between sleep apnea/hypoventilation syndrome and treatment by NIV during hospitalization, it is noteworthy that the numbers of patients undergoing NIV with and without one of these diagnoses were similar. This probably means that relieving acute pulmonary congestion and improving pulmonary gas exchange were the main treatment goals in a large number of those treated with NIV.
Our in-hospital mortality was double (7.9%) that reported in a large European observational survey (3.8%)2 and in a US registry (4.0%)27 but similar to that reported in other Portuguese studies and in Italian and French surveys (7.7%, 6.9% and 8.2%, respectively).4,13,25
Pharmacological treatment at discharge should be considered in the light of the prevalence of HFpEF in this population. Bearing in mind that no drug therapy has been proved to change prognosis in the HFpEF phenotype,5,16 it is interesting to see that half of the patients were prescribed beta-blockers or ACE inhibitors. This proportion is similar to that reported in the OFICA study in the HFpEF subgroup, in which 44.2% and 47.3% of this group of patients were discharged under ACE inhibitors and beta-blockers, respectively.13 This reflects the use of these drug classes in HFpEF patients with the aim of controlling blood pressure and ventricular rate in AF and decreasing hospitalizations. Ceia et al. found that therapy with ACE inhibitors in Portuguese chronic HF patients was also similar between patients with HFpEF and HFrEF.28
Our finding that beta-blockers and spironolactone were more often prescribed for HFrEF patients shows adherence to current guidelines and their incorporation into clinical practice. The rate of such prescription is similar to that in a European survey for beta-blockers (75.2% vs. 80%) but lower for aldosterone blockers (31.2% vs. 52%).2
The total one-year mortality was higher than that reported from the same European region (34.3% vs. 24.7%) by Maggioni et al. in the ESC-HF Pilot survey for the period 2009-2010 and in an Italian survey (24%).2,4 Cardiovascular causes accounted for half of deaths, a smaller proportion than reported in other observational trials, probably because the type of HF patients hospitalized in cardiology departments are more liable to die of cardiovascular causes, while those hospitalized in internal medicine wards are equally likely to die of other causes. In this respect, it is noteworthy that the patients in our study were 10 years older and had a higher prevalence of comorbidities.3,4 Comorbidity was found to be one of the prime determinants of prognosis in a study of patients hospitalized with HF1 and HFpEF patients have a higher likelihood of non-cardiovascular death,6 supporting our findings.
It should be noted that, although it is commonly accepted that the lower the EF the worse the survival,5 in our predominantly HFpEF population neither mortality nor rehospitalization rates were lower. This is in agreement with other hospital-based studies of patients hospitalized with HF that reported similar one-year mortality rates in patients with HFpEF compared to those with HFrEF,1,6 but not with the OFICA study, which reported higher mortality in the HFrEF population.13
The rehospitalization rate for HF in the first year of follow-up was similar in this study to that found for the same European region in the previously mentioned survey (30.5% vs. 33.9%, respectively). Of note, the highest rates of mortality and rehospitalization for HF were observed in this region, in comparison with three other European regions.3,4 Bearing in mind the differences in prevalence of HFpEF, this is in agreement with studies reporting that HFpEF patients are as likely to be rehospitalized as HFrEF patients.6
The median time between discharge and first follow-up appointment was much longer than the recommended 7-14 days,16 a situation that we expect to change drastically with the implementation of our heart failure clinic.
To our knowledge this is the largest Portuguese observational study of patients hospitalized for HF, and the most recent.
Our findings should be considered in the context of several limitations. This was a retrospective registry and did not include all patients hospitalized for HF, including those admitted to the cardiology department of our hospital. Unmeasured variables may have been present that could have influenced the findings. Chronic renal dysfunction was not included in the comorbidities because of the difficulty of ascertaining the chronicity of renal dysfunction in some patients with cardiorenal syndromes. Rehospitalizations were considered only at the study center, and thus may have been underestimated. We did not examine the use of cardiac devices, although there is unlikely to be a significant number of patients with such devices, given the low prevalence of reduced ejection fraction and the old age of this population.
ConclusionsThis is one of the few published observational studies showing the situation in Portugal in terms of HF hospitalization and outcomes. We characterized a large group of patients admitted to an internal medicine department with acute HF: elderly, mostly female, with hypertension and HFpEF. Diabetic patients and those with ischemic heart disease were significantly more likely to have HFrEF. At discharge, more than half of patients were prescribed beta-blockers and ACE inhibitors/ARBs, and those with HFrEF were significantly more often prescribed beta-blockers and spironolactone. Nearly a third of patients died and/or were rehospitalized in the following year.
Multicenter observational studies in the Portuguese HF population are an unmet need. For the time being, the data presented here will be helpful to measure the impact of the heart failure clinic at our institution in important areas, particularly mortality and rehospitalization outcomes.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors wish to thank João Pedro Ferreira for his contribution to the design and data collection for this study and Inês Silveira for data collection.
Novartis Pharma supported the statistical analysis through an unrestricted grant.
Betânia Ferreira is currently an employee of Hospital da Luz Arrábida, Grupo Luz Saúde, Vila Nova de Gaia, Portugal. Sandra Nunes is currently an employee of Centro Hospitalar Entre Douro e Vouga, E.P.E, Santa Maria da Feira, Portugal.







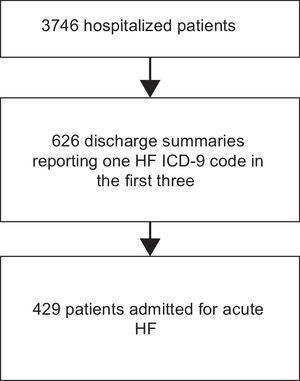 ICD-9: International Classification of Diseases, 9th Revision.' title='Flow diagram of patient enrollment. The data refer to admissions to the internal medicine department in the study period. HF: heart failure;
ICD-9: International Classification of Diseases, 9th Revision.' title='Flow diagram of patient enrollment. The data refer to admissions to the internal medicine department in the study period. HF: heart failure;