Diabetic patients have a 2–4 times higher risk of cardiovascular disease than non-diabetic individuals.
The aims of this study are to evaluate the effects of a cardiac rehabilitation program (phase II) in patients with diabetes and coronary disease and to compare the results with regard to control of cardiovascular risk factors and improvement in functional capacity with coronary patients without diabetes.
MethodsThis was a prospective study of patients diagnosed with ischemic heart disease referred for a cardiac rehabilitation program between January 2009 and June 2013. The population was divided into two groups: diabetic and non-diabetic.
Patients were assessed at the beginning of phase II and three months later and the following parameters were recorded: body mass index, waist circumference, lipid profile, blood glucose and glycated hemoglobin in diabetic patients, blood pressure, smoking, physical activity level (using the International Physical Activity Questionnaire) and functional capacity (on treadmill stress testing).
ResultsThe study population consisted of 682 patients (253 diabetic and 429 non-diabetic). Diabetic patients were significantly older, had a worse cardiovascular risk profile (higher prevalence of overweight, dyslipidemia, hypertension and sedentary lifestyle) and lower functional capacity.
At the end of phase II, there was a statistically significant improvement (p<0.05) in all risk factors and functional capacity, which was similar in both groups, except for body mass index, triglycerides and functional capacity.
ConclusionsDiabetic patients may benefit from a cardiac rehabilitation program and achieve comparable results to non-diabetic patients.
Doentes diabéticos têm um risco de doença cardiovascular duas a quatro vezes superior a não diabéticos. Os objetivos do estudo são: avaliar os efeitos de um programa de reabilitação cardíaca (fase II) em doentes coronários diabéticos e comparar os seus resultados em termos de controlo de fatores de risco cardiovasculares e ganhos na capacidade funcional com doentes coronários não diabéticos.
MétodosEstudo prospetivo integrando doentes com doença cardíaca isquémica orientados para programa de reabilitação cardíaca entre janeiro de 2009 e junho de 2013. Consideraram-se dois grupos: diabéticos e não diabéticos. Foram avaliados na primeira consulta da fase II e três meses depois, com registo dos seguintes parâmetros: índice de massa corporal, perímetro abdominal, perfil lipídico, hemoglobina glicada e glicose nos diabéticos, pressão arterial, tabagismo, nível de atividade física (através do International Physical Activity Questionnaire) e capacidade funcional (alcançada em prova de esforço).
ResultadosAmostra de 682 doentes (253 diabéticos e 429 não diabéticos). Os diabéticos eram significativamente mais idosos, apresentavam pior perfil de risco cardiovascular (maior prevalência de excesso ponderal, dislipidemia, hipertensão arterial e sedentarismo) e menor capacidade funcional. No final da fase II ocorreu uma melhoria estatisticamente significativa (p<0,05) em todos os fatores de risco e na capacidade funcional, que foi semelhante nos dois grupos com exceção do índice de massa corporal, dos triglicerídeos e da capacidade funcional.
ConclusõesDoentes diabéticos podem beneficiar com um programa de reabilitação cardíaca e alcançar resultados comparáveis a não diabéticos.
acute coronary syndrome
body mass index
blood pressure
coronary artery disease
cardiac rehabilitation program
diabetes mellitus
exercise testing
glycated hemoglobin
high-density lipoprotein cholesterol
ischemic heart disease
International Physical Activity Questionnaire
low-density lipoprotein cholesterol
metabolic equivalents
percutaneous coronary intervention
standard deviation
total cholesterol
triglycerides
waist circumference
World Health Organization
Cardiac rehabilitation programs (CRPs) are multidisciplinary interventions that are designed to help cardiac patients achieve and maintain their maximum physical and psychosocial potential.1
CRPs are a valuable therapeutic option that provide multiple benefits by promoting healthy lifestyles and cardiovascular risk factor control, symptom relief and optimization of functional capacity, while reducing the incidence of new cardiovascular events, thus helping patients to return to a productive and satisfying life.2 Studies have reported a 25% reduction in mortality following myocardial infarction (MI) in patients on CRPs compared to those not undergoing cardiac rehabilitation.3,4 However, CRPs continue to be underused in Portugal; according to Diagnosis Related Groups data from 2007 and the 2007 survey of the Portuguese Society of Cardiology's Study Group on Exercise Physiology and Cardiac Rehabilitation, only 3% of patients discharged from hospital after MI were admitted to a CRP, with even lower percentages for other cardiovascular disease.5 In 2007, Portugal was second from last in Europe for cardiac rehabilitation, despite doubling patient numbers compared to 2004.5
The clinical indications for a CRP include acute coronary syndrome (ACS), stable angina, revascularization by percutaneous coronary intervention (PCI) or coronary artery bypass grafting, valve surgery, compensated heart failure and heart transplantation, as well as for control of cardiovascular risk factors in patients at high risk of coronary artery disease (CAD).1,2
CRPs consist of three or four phases, in accordance with the European6 and American7 guidelines, respectively, beginning with admission for a cardiovascular event and ending at the point when the individual patient takes full responsibility for maintaining the strategies learned.
Patients with diabetes mellitus (DM) have a 2–4 times higher risk of cardiovascular disease, particularly CAD, than those without and DM doubles mortality due to a cardiovascular event, even after adjustment for other cardiovascular risk factors.8,9
The World Health Organization (WHO) has declared that DM is a major public health issue, and that it is essential to implement health education measures, given that there are predicted to be 366 million diabetic individuals worldwide by 2030.10 In Portugal, 11.7% of the population aged 20–79 years have diabetes.11
Although mortality from coronary events has fallen in recent decades in the general population as a result of improved control of cardiovascular risk factors and more effective treatment of heart disease, this has not been the case for diabetic patients.12
The approach to reducing cardiovascular risk in diabetic patients includes diet modification, control of cardiovascular risk factors, regular exercise and drug therapy.13 These strategies lead to favorable metabolic and endocrine responses, which in the medium and long term will be reflected in reduced glycated hemoglobin (HbA1c), glucose intolerance and insulin resistance, increased muscle glucose uptake, reduced adipose tissue and increased exercise tolerance. Together, these benefits slow development of the micro- and macrovascular complications associated with DM, thus reducing cardiovascular risk and improving patients’ quality of life.7,13,14
Of patients referred for CRPs, 20–30% have DM,15 but few studies have assessed the efficacy of CRPs specifically in diabetic patients, even though such programs may be especially valuable in this patient population.
The aim of the present study is to evaluate the effects of phase II of a CRP in patients with CAD and type 2 DM and to compare the results with regard to control of risk factors and improvement in functional capacity with coronary patients without diabetes.
MethodsThis was a single-center, prospective, observational cohort study of 818 patients diagnosed with ischemic heart disease (IHD), consecutively referred for a CRP in the Cardiovascular Prevention and Rehabilitation Unit of Hospital de Santo António, Porto, between January 2009 and June 2013. Of the initial sample, 136 patients were excluded, of whom 91 quit the CRP, nine suffered clinical complications that prevented them from completing the minimum of eight sessions (due to rehospitalization for PCI in two, ACS in one, and musculoskeletal lesions in six), and 36 due to lack of data during follow-up, particularly laboratory test results or anthropometric data that were required for the statistical analysis. The study population thus consisted of 682 patients who began the CRP within three months of the event, irrespective of the admission diagnosis. The population was divided into two groups: the diabetic group, composed of patients with a history of type 2 DM (confirmed in their medical records) and those under antidiabetic therapy (oral antidiabetics or insulin therapy), and the non-diabetic group.
The patients underwent two assessments, one at the beginning of the CRP and the second three months later. The first assessment consisted of clinical history, including sociodemographic data and personal and family history, and physical examination of the cardiovascular, musculoskeletal and neurological systems. At both assessments, data were collected on risk profile, including blood pressure (BP), body mass index (BMI) (in kg/m2) and waist circumference (WC), smoking, blood glucose and HbA1c, and lipid profile after 12 hours fasting, consisting of total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C) and triglycerides (TG).
The following were used as reference values: BP <130/80 mmHg in two consecutive measurements; BMI 18–24.9 kg/m2 (BMI 25–29.9 kg/m2 being classified as overweight and BMI ≥30 kg/m2 being classified as obese); WC <80 cm in women and <94 cm in men; fasting capillary glucose <110 mg/dl and HbA1c <6.5%; TC <190 mg/dl, LDL-C <100 mg/dl, HDL-C >45 mg/dl in men and >40 mg/dl in women, and TG <150 mg/dl.
Patients’ level of physical activity was assessed using the International Physical Activity Questionnaire (IPAQ), which has been validated for the Portuguese population16; this is designed to quantify (in metabolic equivalents [METs]/min/week) the amount of exercise taken in a week performing various activities (including household chores, employment, sport and recreation). The following categories were used in the analysis: sedentary lifestyle (<600 METs/min/week); moderate exercise (600–3000 METs/min/week); and vigorous exercise (>3000 METs/min/week).
At each assessment, all patients underwent treadmill exercise testing (ET), under their usual medication, to determine parameters of chronotropic and hemodynamic response. Maximum functional capacity during ET was estimated in METs, based on the metabolic equations of the American College of Sports Medicine for treadmill exercise,7 and total ET time was also recorded.
Cardiac rehabilitation programThe CRP includes individual counseling on strategies for control of cardiovascular risk factors, supervised exercise sessions and group health education sessions.
Supervised exerciseAll patients took part in twice-weekly exercise sessions supervised by a cardiologist, a physiatrist and a physiotherapist. The CRP lasts for 8–12 weeks depending on cardiac risk stratification, absence of complications during the program and patients’ availability based on the distance from their place of residence and need to return to work.
Each session lasts between 60 and 90 minutes; the exercise protocol includes a warm-up period, aerobic training (treadmill and arm and leg ergometers), resistance training (using elastic bands, dumbbells, exercise balls and other strength training equipment), a cool-down period and flexibility exercises. The intensity of aerobic exercise was determined for each individual patient, based on their exercise heart rate calculated by the Karvonen formula17 using the data obtained from ET, and complemented by the patient's rating of perceived exertion on the Borg scale.7
Prior to each exercise session, a brief clinical assessment was performed that included a questionnaire on relevant symptoms and compliance with drug therapy, and measurement of baseline heart rate and BP; capillary glucose was also assessed in diabetic patients. Heart rate was continuously monitored during each session by remote ECG monitoring or heart rate monitor, in accordance with international guidelines on the appropriate level of supervision and monitoring for each patient.7
In addition, patients were encouraged to exercise on the other days of the week in accordance with the guidelines on secondary prevention.7,17
Health educationPeriodic group sessions involving patients and their relatives were held on various subjects, including “Coronary Artery Disease”, “Nutrition”, “Stress” and “Exercise”.
When clinically indicated, patients were referred for specialist consultations in the unit, for endocrinology, psychiatry, smoking cessation, urology or vascular surgery. All diabetic patients were assessed by a nutritionist and prescribed an individualized diet program.
Statistical analysisStatistical analysis of the data was performed using Statistical Package for the Social Sciences (SPSS) version 17.0. Continuous variables are presented as means ± standard deviation (SD) for those with normal distribution and as medians and interquartile range (P25–P75) for those with non-normal distribution. Differences within each patient group were assessed by the Student's t test for paired samples for continuous variables with normal distribution and by the Wilcoxon test for those with non-normal distribution. Differences in CRP response between the groups were assessed by the Student's t test to compare means and by the Mann-Whitney test to compare medians. Categorical variables were compared using the McNemar test for differences within groups and the chi-square test for differences between groups.
Values of p<0.05 were considered statistically significant.
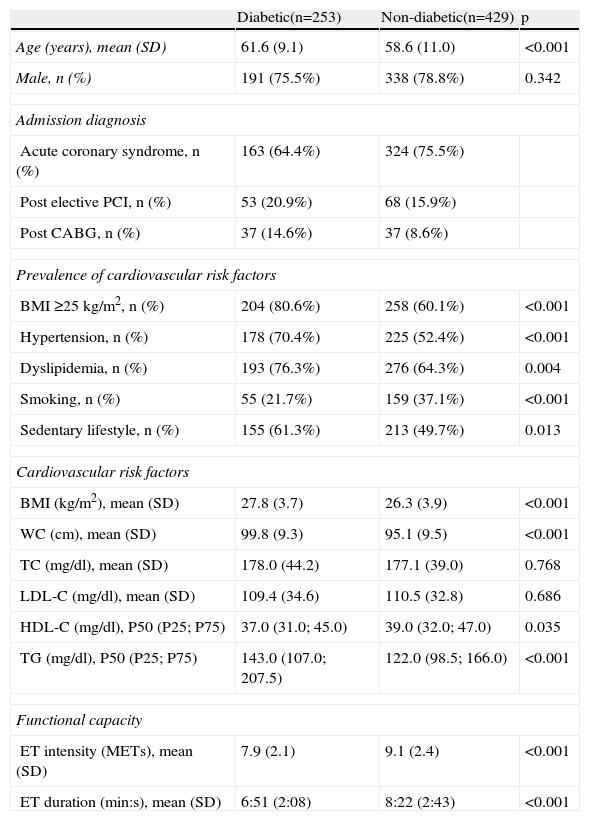
ResultsThe study population consisted of 682 patients (253 diabetic and 429 non-diabetic). Both groups had a higher proportion of males. The most common admission diagnosis in both groups was ACS. Full characterization of the study population on admission to the CRP is shown in Table 1.
Characteristics of the study population on admission to the cardiac rehabilitation program.
| Diabetic(n=253) | Non-diabetic(n=429) | p | |
| Age (years), mean (SD) | 61.6 (9.1) | 58.6 (11.0) | <0.001 |
| Male, n (%) | 191 (75.5%) | 338 (78.8%) | 0.342 |
| Admission diagnosis | |||
| Acute coronary syndrome, n (%) | 163 (64.4%) | 324 (75.5%) | |
| Post elective PCI, n (%) | 53 (20.9%) | 68 (15.9%) | |
| Post CABG, n (%) | 37 (14.6%) | 37 (8.6%) | |
| Prevalence of cardiovascular risk factors | |||
| BMI ≥25 kg/m2, n (%) | 204 (80.6%) | 258 (60.1%) | <0.001 |
| Hypertension, n (%) | 178 (70.4%) | 225 (52.4%) | <0.001 |
| Dyslipidemia, n (%) | 193 (76.3%) | 276 (64.3%) | 0.004 |
| Smoking, n (%) | 55 (21.7%) | 159 (37.1%) | <0.001 |
| Sedentary lifestyle, n (%) | 155 (61.3%) | 213 (49.7%) | 0.013 |
| Cardiovascular risk factors | |||
| BMI (kg/m2), mean (SD) | 27.8 (3.7) | 26.3 (3.9) | <0.001 |
| WC (cm), mean (SD) | 99.8 (9.3) | 95.1 (9.5) | <0.001 |
| TC (mg/dl), mean (SD) | 178.0 (44.2) | 177.1 (39.0) | 0.768 |
| LDL-C (mg/dl), mean (SD) | 109.4 (34.6) | 110.5 (32.8) | 0.686 |
| HDL-C (mg/dl), P50 (P25; P75) | 37.0 (31.0; 45.0) | 39.0 (32.0; 47.0) | 0.035 |
| TG (mg/dl), P50 (P25; P75) | 143.0 (107.0; 207.5) | 122.0 (98.5; 166.0) | <0.001 |
| Functional capacity | |||
| ET intensity (METs), mean (SD) | 7.9 (2.1) | 9.1 (2.4) | <0.001 |
| ET duration (min:s), mean (SD) | 6:51 (2:08) | 8:22 (2:43) | <0.001 |
Values expressed as means (SD) or number (percentage) or median (interquartile range) [P50 (P25; P75)]. BMI: body mass index; CABG: coronary artery bypass grafting; ET: exercise test; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; METs: metabolic equivalents; PCI: percutaneous coronary intervention; SD: standard deviation; TC: total cholesterol; TG: triglycerides; WC: waist circumference.
Diabetic patients were significantly older (61.6±9.1 vs. 58.6±11.0 years, p<0.001) and presented worse cardiovascular risk profiles (Table 1): greater prevalence of overweight (80.6% vs. 60.1%, p<0.001) and significantly higher BMI and WC; greater prevalence of dyslipidemia (76.3% vs. 64.3%, p=0.004) and significantly higher TG and lower HDL-C; and greater prevalence of hypertension (70.4% vs. 52.4%, p<0.001) and sedentary lifestyle (61.3% vs. 49.7%, p=0.013). However, they had a lower prevalence of smoking (21.7% vs. 37.1%, p<0.001). Functional capacity was significantly lower in diabetic patients: 7.9±2.1 METs vs. 9.1±2.4 METs, p<0.001; ET duration: 6:51±2:08 min:s vs. 8:22±2:43 min:s, p<0.001.
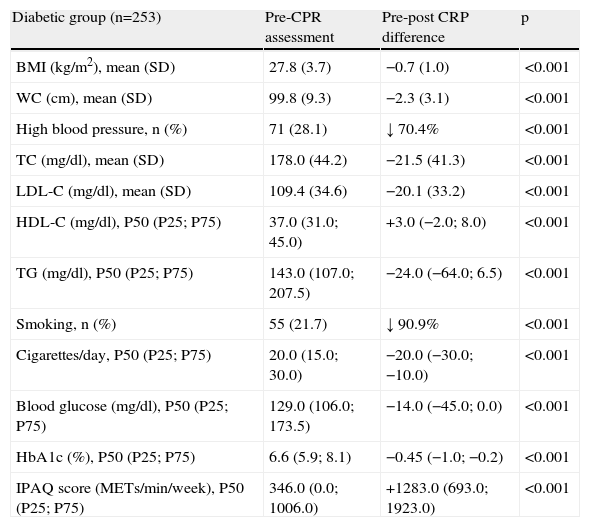
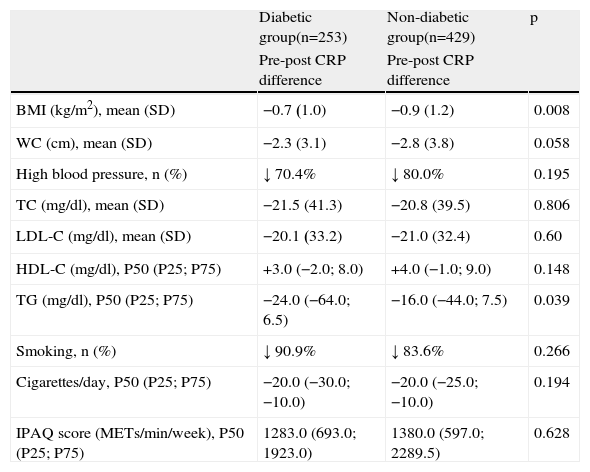
Changes in cardiovascular risk factors over the study period in the diabetic and non-diabetic groups are summarized in Tables 2 and 3, and Table 4 compares these changes between the two groups. Table 5 shows changes in functional capacity in each group, and compares the two groups.
Changes in cardiovascular risk factors after the cardiac rehabilitation program in diabetic patients.
| Diabetic group (n=253) | Pre-CPR assessment | Pre-post CRP difference | p |
| BMI (kg/m2), mean (SD) | 27.8 (3.7) | −0.7 (1.0) | <0.001 |
| WC (cm), mean (SD) | 99.8 (9.3) | −2.3 (3.1) | <0.001 |
| High blood pressure, n (%) | 71 (28.1) | ↓ 70.4% | <0.001 |
| TC (mg/dl), mean (SD) | 178.0 (44.2) | −21.5 (41.3) | <0.001 |
| LDL-C (mg/dl), mean (SD) | 109.4 (34.6) | −20.1 (33.2) | <0.001 |
| HDL-C (mg/dl), P50 (P25; P75) | 37.0 (31.0; 45.0) | +3.0 (−2.0; 8.0) | <0.001 |
| TG (mg/dl), P50 (P25; P75) | 143.0 (107.0; 207.5) | −24.0 (−64.0; 6.5) | <0.001 |
| Smoking, n (%) | 55 (21.7) | ↓ 90.9% | <0.001 |
| Cigarettes/day, P50 (P25; P75) | 20.0 (15.0; 30.0) | −20.0 (−30.0; −10.0) | <0.001 |
| Blood glucose (mg/dl), P50 (P25; P75) | 129.0 (106.0; 173.5) | −14.0 (−45.0; 0.0) | <0.001 |
| HbA1c (%), P50 (P25; P75) | 6.6 (5.9; 8.1) | −0.45 (−1.0; −0.2) | <0.001 |
| IPAQ score (METs/min/week), P50 (P25; P75) | 346.0 (0.0; 1006.0) | +1283.0 (693.0; 1923.0) | <0.001 |
Values expressed as means (SD) or number (percentage) or median (interquartile range) [P50 (P25; P75)]. BMI: body mass index; CPR: cardiac rehabilitation program; HbA1c: glycated hemoglobin; HDL-C: high-density lipoprotein cholesterol; IPAQ: International Physical Activity Questionnaire; LDL-C: low-density lipoprotein cholesterol; METs: metabolic equivalents; SD: standard deviation; TC: total cholesterol; TG: triglycerides; WC: waist circumference.
Changes in cardiovascular risk factors after the cardiac rehabilitation program in non-diabetic patients.
| Non-diabetic group (n=429) | Pre-CPR assessment | Pre-post CRP difference | p |
| BMI (kg/m2), mean (SD) | 26.3 (3.9) | −0.9 (1.2) | <0.001 |
| WC (cm), mean (SD) | 95.1 (9.5) | −2.8 (3.8) | <0.001 |
| High blood pressure, n (%) | 90 (21.0) | ↓ 80.0% | <0.001 |
| TC (mg/dl), mean (SD) | 177.1 (39.0) | −20.8 (39.5) | <0.001 |
| LDL-C (mg/dl), mean (SD) | 110.5 (32.8) | −21.0 (32.4) | <0.001 |
| HDL-C (mg/dl), P50 (P25; P75) | 39.0 (32.0; 47.0) | +4.0 (−1.0; 9.0) | <0.001 |
| TG (mg/dl), P50 (P25; P75) | 122.0 (98.5; 166.0) | −16.0 (−44.0; 7.5) | <0.001 |
| Smoking, n (%) | 159 (37.1) | ↓ 83.6% | <0.001 |
| Cigarettes/day, P50 (P25; P75) | 20.0 (10.0; 30.0) | −20.0 (−25.0. −10.0) | <0.001 |
| IPAQ score (METs/min/week), P50 (P25; P75) | 594.0 (0.0; 1386.0) | +1380.0 (597.0; 2289.5) | <0.001 |
Values expressed as means (SD) or number (percentage) or median (interquartile range) [P50 (P25; P75)]. BMI: body mass index; CPR: cardiac rehabilitation program; HDL-C: high-density lipoprotein cholesterol; IPAQ: International Physical Activity Questionnaire; LDL-C: low-density lipoprotein cholesterol; METs: metabolic equivalents; SD: standard deviation; TC: total cholesterol; TG: triglycerides; WC: waist circumference.
Comparison of changes in cardiovascular risk factors after the cardiac rehabilitation program in the diabetic and non-diabetic groups.
| Diabetic group(n=253) | Non-diabetic group(n=429) | p | |
| Pre-post CRP difference | Pre-post CRP difference | ||
| BMI (kg/m2), mean (SD) | −0.7 (1.0) | −0.9 (1.2) | 0.008 |
| WC (cm), mean (SD) | −2.3 (3.1) | −2.8 (3.8) | 0.058 |
| High blood pressure, n (%) | ↓ 70.4% | ↓ 80.0% | 0.195 |
| TC (mg/dl), mean (SD) | −21.5 (41.3) | −20.8 (39.5) | 0.806 |
| LDL-C (mg/dl), mean (SD) | −20.1 (33.2) | −21.0 (32.4) | 0.60 |
| HDL-C (mg/dl), P50 (P25; P75) | +3.0 (−2.0; 8.0) | +4.0 (−1.0; 9.0) | 0.148 |
| TG (mg/dl), P50 (P25; P75) | −24.0 (−64.0; 6.5) | −16.0 (−44.0; 7.5) | 0.039 |
| Smoking, n (%) | ↓ 90.9% | ↓ 83.6% | 0.266 |
| Cigarettes/day, P50 (P25; P75) | −20.0 (−30.0; −10.0) | −20.0 (−25.0; −10.0) | 0.194 |
| IPAQ score (METs/min/week), P50 (P25; P75) | 1283.0 (693.0; 1923.0) | 1380.0 (597.0; 2289.5) | 0.628 |
Values expressed as means (SD) or number (percentage) or median (interquartile range) [P50 (P25; P75)]. BMI: body mass index; CPR: cardiac rehabilitation program; HDL-C: high-density lipoprotein cholesterol; IPAQ: International Physical Activity Questionnaire; LDL-C: low-density lipoprotein cholesterol; METs: metabolic equivalents; SD: standard deviation; TC: total cholesterol; TG: triglycerides; WC: waist circumference.
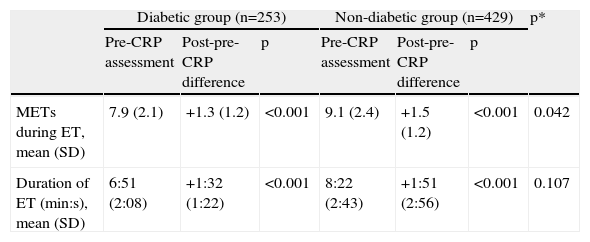
Changes in functional capacity after the cardiac rehabilitation program in each group and comparison between groups.
| Diabetic group (n=253) | Non-diabetic group (n=429) | p* | |||||
| Pre-CRP assessment | Post-pre-CRP difference | p | Pre-CRP assessment | Post-pre-CRP difference | p | ||
| METs during ET, mean (SD) | 7.9 (2.1) | +1.3 (1.2) | <0.001 | 9.1 (2.4) | +1.5 (1.2) | <0.001 | 0.042 |
| Duration of ET (min:s), mean (SD) | 6:51 (2:08) | +1:32 (1:22) | <0.001 | 8:22 (2:43) | +1:51 (2:56) | <0.001 | 0.107 |
Values are expressed as means (SD). CRP: cardiac rehabilitation program; ET: exercise test; METs: metabolic equivalents; SD: standard deviation.
p*: p value comparing the mean of differences between groups in response to the cardiac rehabilitation program.
Overweight was the most prevalent cardiovascular risk factor in the diabetic group (80.6%), of whom 22.9% were obese.
Both groups showed improved anthropometric parameters over the course of the CRP (Tables 2 and 3). The improvement was similar in the two groups for WC (p=0.058) but not for BMI, the mean decrease in BMI being significantly greater in absolute terms in the non-diabetic group (p=0.008).
HypertensionOn admission to the CRP, 70.4% of diabetic and 52.4% of non-diabetic patients had a history of hypertension. At the first assessment, 28.1% of the diabetic group and 21.0% of the non-diabetic group presented high BP. Following the CRP, there was a significant decrease in the number of patients in both groups with uncontrolled BP (decrease of 70.4%, p<0.001, in the diabetic group and 80.0%, p<0.001, in the non-diabetic group), with a non-significant difference between the groups (p=0.195).
DyslipidemiaDyslipidemia was the most common cardiovascular risk factor among non-diabetic patients (64.3%).
At the end of phase II of the CRP, an improved lipid profile was seen in both groups, reflected in both a significant decrease in TC, LDL-C and TG and a significant increase in HDL-C (Tables 2 and 3).
Changes in the various lipid parameters following the CRP were similar in both groups, except for the decrease in TG, which in absolute terms was significantly greater in diabetic patients (p=0.039).
SmokingOn admission to the program, 21.7% of the diabetic group and 37.1% of the non-diabetic group were smokers. At the end of phase II, there was a 90.0% reduction in the number of smokers in the diabetic group (p<0.001) and an 83.6% reduction in the non-diabetic group (p<0.001), a similar decrease in both groups (p=0.266).
There was also a significant reduction in the number of cigarettes per day (Tables 2 and 3), with no significant difference between the groups (p=0.194).
Diabetes mellitusDiabetic patients showed improved control of DM following the CRP, reflected in significant reductions in fasting glucose and HbA1c (Table 2).
Sedentary lifestyleAt the beginning of the study, 61.3% of the diabetic group and 49.7% of the non-diabetic group had sedentary lifestyles, as shown by their IPAQ scores.
Both groups showed significantly increased levels of physical activity over the course of the CRP, as expressed by their weekly exercise measured by the IPAQ (Tables 2 and 3). The increase in IPAQ scores was similar in the two groups (p=0.628).
Functional capacityAt the start of the study, diabetic patients presented worse functional capacity (Table 1). By the end of the CRP, both groups showed significant improvement in mean METs (+1.3 [1.2], p<0.001, in the diabetic group vs. +1.5 [1.2], p<0.001, in the non-diabetic group) and in ET duration (+1:32 [1:22] min:s, p<0.001, in the diabetic group vs. +1:51 [2:56] min:s, p<0.001, in the non-diabetic group) (Table 5). There was a significantly smaller improvement in functional capacity in the diabetic group in terms of METs (p=0.042), as well as in ET duration, although without statistical significance in the latter (p=0.107) (Table 5).
DiscussionThe metabolic abnormalities that characterize DM, particularly hyperglycemia, increased free fatty acids and insulin resistance, lead to changes at the molecular level that result in decreased availability of nitric oxide and increased oxidative stress, which in turn lead to vascular dysfunction.18 This accelerates atherosclerosis and thereby increases cardiovascular risk in diabetic patients.
In 1997, the WHO considered overweight and obesity to be a rising epidemic, associated with five of the ten leading causes of death in industrialized countries: DM, IHD, stroke, atherosclerosis and some forms of cancer.19 Obesity raises the risk of CAD, probably due to the adverse metabolic changes resulting from increased abdominal fat that play a central role in peripheral insulin resistance.20
There was a high prevalence of overweight and obesity in our study population, particularly in those with type 2 DM. The sedentary lifestyle found in 61.3% of the diabetic group may also have been a contributing factor.
Unlike in other studies21,22 in which BMI did not fall significantly in diabetic patients, there was a significant decrease in BMI and WC in both groups by the end of phase II of the CRP. This may be due to the individualized assessment and counseling provided by a nutritionist in our program. In addition, all patients were given an individual exercise plan, although no specific measures were prescribed for obese patients.
Hypertension and type 2 DM are frequently found together, which further increases the already higher cardiovascular risk of diabetic patients. The prevalence of hypertension in patients with diabetes is higher than in the general population (40–60% in those aged 45–75 years).23 In our population, 70.4% of the diabetic group and 52.4% of the non-diabetic group presented hypertension, in agreement with other studies.24,25
Control of hypertension in diabetic patients is an essential preventive measure, since it reduces micro- and macrovascular complications, and target BP levels should be lower than in non-diabetic patients.26 Each 10-mmHg decrease in systolic BP is associated with an average 12% reduction in diabetes-related complications, particularly cardiovascular disease.27
At the initial assessment, 28.1% of the diabetic group and 21.0% of the non-diabetic group presented elevated BP, and thus most patients had controlled BP at the start of the CRP. This may be because most were under optimized antihypertensive therapy, having been referred following hospitalization in the cardiology department. There was a statistically significant decrease in the number of patients with uncontrolled hypertension over the study period. The benefits of regular aerobic exercise by lowering BP in hypertensive patients are well documented in the literature.28,29 Nevertheless, the pathophysiological mechanisms underlying the antihypertensive effects of exercise are the subject of debate. Some studies report reductions in total peripheral resistance, sympathetic nerve activity and plasma norepinephrine levels,29,30 while according to others there is increased total peripheral resistance in the post-exercise recovery period, associated with a significant decrease in cardiac output.29,31 Improved endothelial function following exercise may also contribute to its antihypertensive effect.29,32
The lipid profile in patients with type 2 DM is usually characterized by hypertriglyceridemia and low HDL-C. LDL-C levels are often similar to those in non-diabetic individuals, but LDL particles are generally smaller and denser in diabetic patients and hence highly atherogenic, so even though LDL-C concentrations are similar, the rates of CAD are higher in diabetic patients.33
Appropriate treatment of dyslipidemia can lead to significant reductions in cardiovascular morbidity and mortality in diabetic patients.20 Studies have demonstrated that for each 1% increase in HDL-C levels, IHD progression decreases by around 3%.34 A meta-analysis assessing the effects of aerobic exercise on the lipid profile of patients with type 2 DM compared to controls found that exercise improved all lipid parameters, although only the decrease in LDL-C was statistically significant.35 In our study population, the diabetic group presented a higher prevalence of dyslipidemia, with significantly higher TG and lower HDL-C values.
Favorable changes in all lipid parameters were seen in both groups over the study period; there was a significantly greater fall in TG levels in the diabetic group, which may be explained by the fact that the initial approach to hypertriglyceridemia is blood glucose control,36 and this improved significantly in the diabetic group. Furthermore, all diabetic patients received individualized nutritional counseling, which stressed the importance of reducing saturated fat intake, in accordance with the American Diabetes Association guidelines.36
Smoking is a major independent risk factor for micro- and macrovascular complications in DM, especially among women, and so smoking cessation has a far greater impact in diabetic than in non-diabetic patients.13 By the end of the study, there had been a striking reduction in both the number of smokers and the number of cigarettes per day for those who continued to smoke, which highlights the importance of CRPs in encouraging smoking cessation. However, caution is needed in interpreting these results given the short follow-up period of the study, less than the minimum six months’ abstinence used to define successful smoking cessation.
Blood glucose control is essential in diabetic patients to reduce the risk of cardiovascular disease, since there is an exponential relationship between fasting glucose and the incidence of cardiovascular events.37 There was a significant decrease in fasting glucose and HbA1c in the diabetic group, reflecting better DM control following the CRP. Structured aerobic exercise and resistance training reduce HbA1c by 0.4–0.6%38,39; each 1% fall in HbA1c leads to a 15–20% reduction in the incidence of major cardiovascular events.40 The benefits for glycemic control are even greater if aerobic exercise is combined with resistance training.41
High levels of physical activity are associated with reductions in cardiovascular risk and total mortality decreases by 20–30% for every 4184 kJ/week of energy expenditure.42 In our study, weekly physical activity levels as assessed by the IPAQ increased significantly and by a similar amount in both groups, which was an unexpected finding, given that most patients with type 2 DM are less physically active than non-diabetic individuals, probably due to their higher incidence of physical limitations, lower exercise tolerance and heightened perception of discomfort during exercise.43 It is thus essential to implement measures that promote higher levels of physical activity.
The diabetic group in our study had lower functional capacity as assessed in METs than the non-diabetic group, in agreement with other studies.21,22,24,44–46 Even in the absence of complications, they present reduced peak oxygen uptake for their age and BMI.24 Hyperglycemia is associated with increased stiffness of the great vessels, including the aorta, which reduces coronary artery blood flow and myocardial work capacity, and therefore overall exercise capacity.44 The less favorable anthropometric profile of diabetic patients, together with left ventricular dysfunction and impairment of cardiac autonomic regulation, contributes to their lower exercise capacity.44
Both groups in our study showed significant improvement in functional capacity during the CRP, albeit less marked in the diabetic group. There are conflicting results in the literature concerning gains in exercise capacity in diabetic and non-diabetic patients. Some studies agree with our results, demonstrating improvement in diabetic patients which, while significant, is less pronounced than in non-diabetic individuals.45,46 However, others have reported significant gains that are similar in both patient groups.21,22,24,44,47 This discrepancy may be due to various factors, such as differences in the participants’ baseline characteristics (age, medication, disease severity, prevalence of comorbidities and exercise intensity) or differences in compliance with the exercise program or its duration.
In the studies reporting less marked improvement in functional capacity in diabetic patients with CRPs, the reasons remain unclear, although it has been suggested that hyperglycemia plays an important role.48 Other mechanisms may also contribute. Insulin is an important regulator of muscle proteins, stimulating the synthesis of mitochondrial proteins, and patients with type 2 DM generally present dysfunction of mitochondria in skeletal muscle. Given that peripheral muscle activity is the main factor governing exercise capacity, mitochondrial dysfunction may explain diabetic patients’ altered response to exercise.48 Moreover, 42% of diabetic patients with no clinical evidence of peripheral vascular disease present significant lower-limb perfusion abnormalities, probably due to microvascular disease, which could also reduce the effect of cardiac rehabilitation on functional capacity.49
The present study found an overall improvement in all parameters related to control of cardiovascular risk factors, as well as in functional capacity; the benefits derived from the CRP were similar in the diabetic group and the non-diabetic group in terms of reducing cardiovascular risk.
This is the first study in Portugal to compare the results of a CRP in diabetic and non-diabetic patients in a large population sample.
The learning process that takes place during the various sessions of the CRP encourages self-control of DM and self-discipline in maintaining a healthy lifestyle, together with self-monitoring of the possible complications and consequences of exercise on the clinical condition of diabetic patients.
Study limitationsThe absence of a control group is a limitation as this would have enabled the natural evolution of the disease to be taken into account, but since comparative studies of usual care versus cardiac rehabilitation have consistently demonstrated the benefits of CRPs,50 we are convinced that the favorable results found in both groups can be attributed specifically to the program.
Another limitation is the short follow-up (three months), and so it is important to perform a long-term assessment.
ConclusionsThe number of diabetic patients in CRPs is increasing, a trend that is likely to continue in view of the predicted rise in the prevalence of DM.
The results of this study demonstrate that patients with type 2 DM may benefit from a CRP and achieve comparable results to non-diabetic patients in terms of improvements in their cardiovascular risk profile.
Diabetic patients are at increased risk of cardiovascular events and thus need more aggressive secondary prevention measures. We therefore emphasize the importance of systematically referring diabetic patients to CRPs given their proven benefits in improving their quality of life.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Toste S, Viamonte S, Barreira A, et al. Reabilitação cardíaca em doentes coronários com diabetes mellitus tipo 2: Estudo comparativo. Rev Port Cardiol. 2014;33:599–608.