Sudden cardiac death (SCD) plays an important part in all-cause mortality in patients infected with human immunodeficiency virus (HIV). The T-peak to T-end (Tp-e) interval, corrected Tp-e (Tp-ec) interval, and Tp-e/QT ratio on the ECG are parameters used to stratify risk for SCD. The objective of this study was to investigate the differences between HIV-infected patients and healthy individuals in terms of Tp-e interval, Tp-ec interval, and Tp-e/QT ratio, as well as other influencing factors.
MethodsNinety-eight HIV-infected patients and 62 healthy controls were included in this prospective case-control study. Tp-e interval, Tp-ec interval, and Tp-e/QT ratio were measured in all participants. Echocardiographic examination and routine laboratory analysis were performed. In addition, CD4 T-cell count and HIV RNA levels were assessed in HIV-infected patients.
ResultsAll baseline characteristics were comparable in both groups. The median survival of those living with HIV was 20.63 months; 53% of them had controlled viral load, and 74% were receiving antiretroviral therapy. Mean baseline CD4 T-cell count was 409. In HIV-infected patients, the Tp-e interval and Tp-ec interval were prolonged, and the Tp-e/QT ratio was higher (p<0.001, p<0.001 and p=0.021, respectively). In bivariate and partial correlation analyses, there was a negative correlation between CD4 T-cell level and Tp-e interval, Tp-ec interval, and Tp-e/QT ratio.
ConclusionTp-e interval, Tp-ec interval, and Tp-e/QT ratio were greater in HIV-infected patients compared with healthy individuals. HIV-infected patients, particularly those with low baseline CD4 T-cell counts, should be closely monitored due to risk of SCD.
A morte súbita cardíaca (MSC) tem um papel importante na mortalidade global dos doentes infetados com VIH. No ECG, o intervalo Tp-e, o intervalo Tp-ec e a relação Tp-e/QT são parâmetros utilizados para a MSC. O objetivo deste estudo consistiu na análise da diferença entre doentes infetados com VIH e indivíduos saudáveis relativamente ao intervalo Tp-e, ao intervalo Tp-ec, à relação Tp-e/QT e aos fatores determinantes.
MétodosNoventa e oito doentes infetados com VIH e 62 indivíduos saudáveis foram incluídos neste estudo caso-controlo prospectivo. O intervalo Tp-e, o intervalo Tp-ec e a relação Tp-e/QT foram medidos em todos os participantes. Foi realizado um exame ecocardiográfico e foram registadas análises laboratoriais de rotina. Além disso, a contagem de células CD4 T e os níveis de VIH-RNA foram avaliados nos doentes infetados com VIH.
ResultadosTodas as características basais foram comparáveis em ambos os grupos. A sobrevivência média das pessoas com VIH foi de 20,63 meses; 53% dos doentes tiveram a carga viral sob controlo e 74% dos mesmos receberam terapêutica antiretroviral. A média da contagem das células T CD4 basais foi de 409. Nos doentes infetados com VIH, o intervalo Tp-e e o intervalo Tp-ec foram prolongados e a relação Tp-e/QT foi superior (p<0,001, p=0,021, respetivamente). Nas análises de correlação bivariada e parcial, houve uma correlação negativa entre o nível das células CD4 T e o intervalo Tp-e, o intervalo Tp-ec e a relação Tp-e/QT.
ConclusãoO intervalo Tp-e, o intervalo Tp-ec e a relação Tp-e/QT foram mais elevados nos doentes infetados com VIH do que nos indivíduos saudáveis. Os doentes infetados com VIH, sobretudo os que apresentam valores baixos na contagem das células T CD4 basais, devem ser rigorosamente monitorizados devido ao risco de MSC.
Now that survival is prolonged in HIV-infected patients, cardiovascular disease has gained importance in this population.1 Cardiovascular disease is 1.5-2 times more common among HIV-infected patients than among noninfected individuals2 and is the leading cause of sudden cardiac death (SCD), which accounts for most cardiac and many non-acquired immunodeficiency syndrome (AIDS)-related natural deaths in HIV-infected patients.3 The sudden death rate is approximately 13% among HIV-infected patients, and 86% of these cases have a cardiac origin. SCD accounted for 86% of all cardiac deaths in a study by Tseng et al.4 In addition, SCD is 4.5 times more common among HIV-infected patients than in noninfected individuals.4 The etiology of SCD in this patient population is not fully understood, however chronic inflammation and immune deficiency may be among its causes.5 In HIV-infected individuals, there is a negative correlation between increases in CD4 T-cell levels and non-AIDS-related mortality.6
In recent years, the Tp-e interval, the interval between the peak and the end of the T wave, has been considered an index of dispersion of ventricular repolarization.7 A prolonged Tp-e interval may be associated with arrhythmogenesis, SCD, and cardiovascular mortality.7,8 In addition to the Tp-e interval, two new parameters, corrected Tp-e interval (Tp-ec) and Tp-e/QT ratio, have been found to be associated with cardiac arrhythmias.9
The objective of this study was to investigate the differences in SCD-related markers (Tp-e interval, Tp-ec interval and Tp-e/QT ratio) between healthy individuals and HIV-infected patients.
MethodsStudy populationThis was a prospective, single-center, case-controlled study. Data were collected from a total of 98 HIV-infected patients and 62 age- and gender-matched healthy volunteers in the referral hospital. Patients were excluded from the study if they had a history of coronary artery disease, atrial fibrillation or flutter, cancer, thyroid dysfunction, or obstructive lung disease.
The ethics committee of Sisli Hamidiye Etfal Educational and Research Hospital approved the study protocol, which was conducted in accordance with the principles of the Declaration of Helsinki on Good Clinical Practice. Written informed consent was obtained from both groups of participants.
Electrocardiographic assessmentA 12-lead electrocardiogram (paper speed 50 mm/s and amplitude 10 mm/mV) was recorded for all participants and assessed by two experienced cardiologists who were blinded to the participants’ demographic parameters. QRS duration, QT interval, and Tp-e interval were measured manually. The Tp-e interval was defined as the interval from the peak to the end of the T wave and measured in leads V2 and V5. The end of the T wave was defined as the point of intersection of the isoelectric line with the line passing through the T wave. The QT interval and Tp-e interval were corrected using Bazett's formula.10 The Tp-e/QT ratio was calculated from these measurement. Intra- and interobserver coefficients of variation were 1.4% and 2.1%, respectively.
Echocardiographic measurementsEchocardiographic (ECG) data were obtained and analyzed by two cardiologists who were unaware of the participants’ subgroups. All echocardiographic measurements were performed on a Philips EPIQ 7 ultrasound machine (Philips Healthcare Inc., Andover, MA, USA) equipped with an S5-1 (1.6-3.2 MHz) transducer. Single-lead ECG recordings were obtained simultaneously. Two-dimensional, M-mode, and color flow Doppler echocardiograms were obtained according to the guidelines.11
Left ventricular ejection fraction (LVEF) was calculated by the biplane Simpson method in apical 4-chamber view. Left ventricular end-diastolic dimension (LVEDd), interventricular septum thickness (IVS), and left ventricular posterior wall thickness (LVPW) were measured at the level of the mitral valve in parasternal long-axis view. Tricuspid annular plane systolic excursion (TAPSE) was measured using M-mode echocardiography in apical 4-chamber view to determine lateral tricuspid annulus motion. Peak velocities of early (E) and late (A) waves were determined from transmitral flow velocity in apical 4-chamber view. Tissue Doppler velocity was measured during early diastole (E′) at the septal and lateral margins of the mitral annulus in apical 4-chamber view, and the E/A and E/E′ ratios were calculated from these measurements. Left ventricular mass (LVM) was calculated according to the Devereux formula.12 Left ventricular mass index (LVMI) was obtained by dividing body surface area by LVM.
Laboratory testingBiochemical tests (hemogram, fasting blood glucose, blood urea, creatinine, low-density lipoprotein [LDL], high-density lipoprotein [HDL], triglycerides and thyroid-stimulating hormone [TSH]) were performed on blood samples taken after 12 hours of fasting. Hemogram, biochemical parameters, and TSH were analyzed by impedance, photometric, and immunoassay methods, respectively. HIV was identified by enzyme-linked immunosorbent assay (ELISA), and a positive result was confirmed by a Western blot test on a blood specimen. HIV RNA was measured using the COBAS AmpliPrep/COBAS TaqMan HIV-1 Test (Roche Molecular Systems, Branchburg, NJ, USA). The results were based on values at the time of enrollment. Controlled HIV was defined as <50 copies/ml and uncontrolled HIV was defined as ≥50 copies/ml. In addition, CD4 T-cell counts were calculated using a Facscan flow cytometer (Becton Dickinson, San Jose, CA, USA). In patients on antiretroviral therapy (ART) the last CD4 counts before ART was initiated were considered, while CD4 T-cell counts for HIV-infected patients who were ART-naive were obtained at the time of enrollment.
Statistical analysisSPSS 16 software (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. Homogeneity of the sample distribution was assessed by the Kolmogorov-Smirnov test. Continuous variables were compared between the two groups with an independent samples t test or the Mann-Whitney U test. Normal distributions are shown as means ± standard deviation and non-normal distributions as medians. Categorical data were compared using the chi-square test or Fisher's exact test and reported as percentages. Spearman's or Pearson's correlation coefficients were used to assess the relationships between continuous variables. Bivariate and partial correlation analyses were performed, the latter between CD4 T-cell counts and Tp-e interval, Tp-ec interval, and Tp-e/QT ratio and controlled TSH and LVEF. A p-value of <0.05 was considered statistically significant. Coefficient of variation analyses were performed to assess intra- and interobserver reproducibility of the ECG data.
ResultsThe clinical and demographic characteristics and the laboratory findings of both groups are shown in Table 1. There were no significant differences between the groups with respect to age, gender, body mass index (BMI), systolic and diastolic blood pressure, fasting blood glucose, total cholesterol, and LDL (p>0.05 for all). Triglycerides were lower in HIV-infected patients compared with controls (p=0.018). The median duration of HIV infection was 20.63 months (range: 1-96). Viral load was under control in 53% of HIV-infected patients, of whom 74% were receiving ART, consisting of protease inhibitors, non-nucleoside reverse transcriptase inhibitors, and integrase inhibitors (11%, 3%, and 59%, respectively). The mean CD4 T-cell count was 409.03 cells/mm3.
Clinical, demographic and laboratory parameters in patients with or without human immunodeficiency virus.
| HIV-infected (n=98) | Controls (n=62) | p | |
|---|---|---|---|
| Age, years | 37.22±10.33 | 35.82±10.04 | 0.399 |
| Male, n (%) | 90 (92) | 55 (89) | 0.582 |
| BMI, kg/m2 | 24.25±3.20 | 24.96±2.79 | 0.152 |
| SBP, mm Hg | 108.218±13.15 | 107.42±10.43 | 0.672 |
| DBP, mm Hg | 66.89±9.10 | 65.32±8.24 | 0.273 |
| Calcium, mg/dl | 9.48±0.31 | 9.56±0.31 | 0.121 |
| Creatinine, mg/dl | 0.91±0.16 | 0.89±0.13 | 0.478 |
| TSH, μIU/ml | 1.57 (1.09-2.21) | 1.59 (1.15-2.31) | 0.829 |
| Total cholesterol, mg/dl | 174.80±41.96 | 178.34±41.10 | 0.600 |
| LDL, mg/dl | 108.92±35.33 | 104.98±37.85 | 0.505 |
| Triglycerides, mg/dl | 116.88±63.01 | 145.17±77.67 | 0.018 |
| Viral load <50 copies/ml, n (%) | 52 (53) | - | - |
| Duration of HIV, months | 20.63 (1-96) | - | - |
| ART use, n (%) | 72 (74) | - | - |
| CD4 T cell count, cells/mm3 | 409.03±182.32 | - | - |
| Duration of ART use, months | 11.13 | - | - |
| Protease inhibitors, n (%) | 11 (11) | - | - |
| NNRTIs, n (%) | 3 (3) | - | - |
| Integrase inhibitors, n (%) | 58 (59) | - | - |
ART: antiretroviral therapy; BMI: body mass index; DBP: diastolic blood pressure; LDL: low-density lipoprotein; HIV: human immunodeficiency virus; CD: cluster of differentiation; NNRTIs: non-nucleoside reverse transcriptase inhibitors; SBP: systolic blood pressure; TSH: thyroid-stimulating hormone;.
Complete ECG and echocardiographic parameters are displayed in Table 2. The groups showed no significant differences in LVEDd, IVS, TAPSE, A and E velocity, LVEF, LV mass index, or resting heart rate. Differences were seen in E/A ratio, corrected QT interval (QTc), Tp-e interval, Tp-ec interval, and Tp-e/QT ratio (p=0.007, p=0.027, p<0.001, p<0.001, and p=0.021, respectively).
Echocardiographic and electrocardiographic parameters in patients with or without human immunodeficiency virus.
| HIV-infected | Controls | p | |
|---|---|---|---|
| LVEDd, mm | 48.74±4.07 | 48.95±3.86 | 0.743 |
| IVS, mm | 8.64±1.24 | 8.68±1.42 | 0.859 |
| LVPW, mm | 8.68±1.22 | 8.61±1.25 | 0.723 |
| TAPSE, mm | 21.47±2.14 | 21.53±2.03 | 0.865 |
| E velocity, cm/s | 80.88±14.14 | 84.54±11.76 | 0.093 |
| A velocity, cm/s | 72.99±16.91 | 68.52±13.24 | 0.066 |
| E’ velocity, cm/s | 14.40±3.50 | 14.52±3.15 | 0.826 |
| E/A ratio | 1.15±0.27 | 1.27±0.26 | 0.007 |
| S, cm/s | 11.74±2.63 | 11.08±2.17 | 0.087 |
| LVEF, % | 58.88±2.39 | 59.36±2.42 | 0.224 |
| LVM index, g/m2 | 76.68±15.74 | 76.70±17.01 | 0.993 |
| Resting HR, bpm | 76.96±10.56 | 74.02±11.85 | 0.104 |
| QTc interval, ms | 398.74±19.74 | 391.08±23.30 | 0.027 |
| Tp-e interval, ms | 84.32±8.68 | 80.03±5.92 | <0.001 |
| Tp-ec interval, ms | 95.20±11.52 | 88.48±7.96 | <0.001 |
| Tp-e/QT ratio | 0.238 | 0.233 | 0.021 |
A: late diastolic mitral inflow velocity; E: early diastolic mitral inflow velocity; E’: early diastolic mitral annular velocity; HR: heart rate; IVS: interventricular septum thickness; LVEDd: left ventricular end-diastolic diameter; LVEF: left ventricular ejection fraction; LVMI: left ventricular mass index; LVPW: left ventricular posterior wall thickness; S: systolic velocity; TAPSE: tricuspid annular plane systolic excursion; Tp-e: T-peak to T-end interval; Tp-ec: corrected Tp-e.
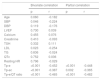
Bivariate and partial correlation analyses are displayed in Table 3. Tp-e interval, Tp-ec interval, and Tp-e/QT ratio were negatively correlated with CD4 T-cell counts.
Correlation of CD4 T cell levels with clinical, laboratory, electrocardiographic and echocardiographic parameters.
| Bivariate correlation | Partial correlation | |||
|---|---|---|---|---|
| p | r | p | r | |
| Age | 0.060 | -0.182 | ||
| SBP | 0.046 | -0.224 | ||
| DBP | 0.119 | -0.176 | ||
| LVEF | 0.730 | 0.039 | ||
| Calcium | 0.455 | 0.076 | ||
| Creatinine | 0.410 | -0.093 | ||
| TSH | 0.332 | 0.111 | ||
| LDL | 0.023 | -0.254 | ||
| TG | 0.836 | -0.024 | ||
| QTc | 0.752 | 0.036 | ||
| Resting HR | 0.796 | -0.029 | ||
| Tp-e | <0.001 | -0.452 | <0.001 | -0.448 |
| Tp-ec | <0.001 | -0.387 | 0.002 | -0.365 |
| Tp-e/QT ratio | <0.001 | -0.465 | <0.001 | -0.482 |
DBP: diastolic blood pressure; HR: heart rate; LDL: low-density lipoprotein; LVEF: left ventricular ejection fraction; QTc: corrected QT interval; SBP: systolic blood pressure; TG: triglycerides; Tp-e: T-peak to T-end interval; Tp-ec: corrected Tp-e; TSH: thyroid-stimulating hormone.
In this study, a prolonged QTc interval, Tp-e interval, and Tp-ec interval were detected in HIV-infected patients compared with healthy individuals. Moreover, the Tp-e/QT ratio was higher in HIV-infected patients. In addition, there was a reverse correlation between CD4 T-cell count and Tp-e interval, Tp-ec interval and Tp-e/QT ratio in HIV-infected patients. To the best of to our knowledge, this is the first study on this topic in the literature.
Thanks to the advent of highly active antiretroviral therapy, which has significantly decreased mortality due to AIDS in HIV-infected patients, most mortality in these patients is now non-AIDS-related.13 Cardiovascular events are the most important cause of non-AIDS-related mortality.14 In a study by Mongardon et al.,15 cardiovascular disease was the second most common cause of cardiac arrest in HIV-infected patients. In the Data Collection on Adverse Events of Anti-HIV Drugs (DAD) study, 16 of the 36 patients with fatal myocardial infarction were diagnosed with an unclassifiable coronary event,16 while in the Strategies for Management of Antiretroviral Therapy (SMART) study, a strong correlation was detected between inflammatory and immunological processes, cardiovascular events, and unwitnessed death.6 Furthermore, chronic HIV-related inflammation has been shown to be related to all-cause mortality and acute myocardial infarction.5
A study by Achhra et al.17 demonstrated that low CD4 T-cell levels predict non-AIDS mortality in HIV-infected patients. In the study by Tseng et al.,4 victims of SCD had mild immunodeficiency. In the SMART study, it was demonstrated that all-cause mortality decreased when the CD4 T-cell count was over 350.18 The relationship between decreased CD4 T-cell count and cardiovascular events and SCD in HIV-infected patients is not fully established. However, endothelial dysfunction caused by HIV, and abnormal calcium release from cardiac cells caused directly by HIV infection, are thought to be responsible for arrhythmias and premature deaths.5,19 Moreover, the direct impact of HIV infection on cardiac repolarization may be another cause of cardiovascular events.20 In populations that are at high risk for SCD, such as HIV-infected patients, new markers are needed.
Tp-e as measured on the ECG, which is inexpensive and easily accessible, has recently become a popular marker.7 Prolongation of the Tp-e interval can be used to predict SCD21 and has been shown to be related to malignant arrhythmias in certain conditions.22
In addition to the Tp-e interval, there is evidence that the Tp-ec interval and Tp-e/QT ratio are more sensitive indicators of increased dispersion of ventricular repolarization and arrhythmogenesis.9 It has also been reported that the above-mentioned markers are more sensitive indicators of arrhythmogenesis than QT dispersion.23 Sauer et al.24 showed that the Tp-e interval reflected electromechanical coupling of dispersion of repolarization in patients with diastolic dysfunction but no other cardiovascular disorder. Another study demonstrated a possible correlation between myocardial contraction time and Tp-e interval.25 There are limited data on the impact of Tp-e interval on heart rate. However, Tp-ec interval, corrected for heart rate using Bazett's formula, has proved more sensitive for predicting SCD.7
In our study, Tp-e interval, Tp-ec interval, and Tp-e/QT ratio were found to be increased in HIV-infected patients compared with healthy individuals. We believe that HIV-infected patients, particularly those who have low CD4 T-cell counts, may have a higher risk of arrhythmias and SCD compared with the normal population.
Study limitationsAlthough Tp-e interval, Tp-ec interval, and Tp-e/QT ratio are sensitive markers for ventricular arrhythmias, the lack of tests on normal hearts and HIV-infected hearts may be considered a limitation of this study. Second, the study group was not followed up for the development of arrhythmias. Finally, measurement of CD4 T-cell levels in HIV-infected patients only might be considered another limitation.
ConclusionHIV-infected patients may be at higher risk of SCD and arrhythmias compared with healthy individuals. In this patient group, the risks of SCD and arrhythmias should be taken into consideration if the Tp-e interval and Tp-ec interval are prolonged and the Tp-e/QT ratio is increased. Long-term follow-up studies dealing with this issue are needed.
Conflicts of interestThe authors have no conflicts of interest to declare.