We report the case of a 21-year-old man who underwent appendectomy under general anesthesia and developed acute pulmonary edema immediately after extubation. We then review the literature, focusing on the pathophysiology and the most important aspects of diagnosis and treatment of post-extubation pulmonary edema.
Apresentamos o caso de um homem de 21 anos, que foi submetido a apendicectomia sob anestesia geral e que imediatamente após a extubação desencadeou quadro de edema pulmonar agudo. A propósito, faremos uma breve revisão da literatura, enfatizando os mecanismos fisiopatológicos subjacentes e os aspectos mais importantes do diagnóstico e tratamento.
Although acute pulmonary edema (APE) as a complication of extubation is uncommon, it has been well characterized. It occurs most frequently in young healthy individuals in the period immediately after extubation, and its severity can worsen the prognosis of low-risk surgery, require invasive treatment and delay hospital discharge1-3. The high negative intrathoracic pressure generated by forceful inspiration against the closed glottis is assumed to be the main pathophysiological mechanism behind this form of APE1,3. This potentially fatal complication is described in a young, previously healthy adult who underwent appendectomy under general anesthesia for acute appendicitis.
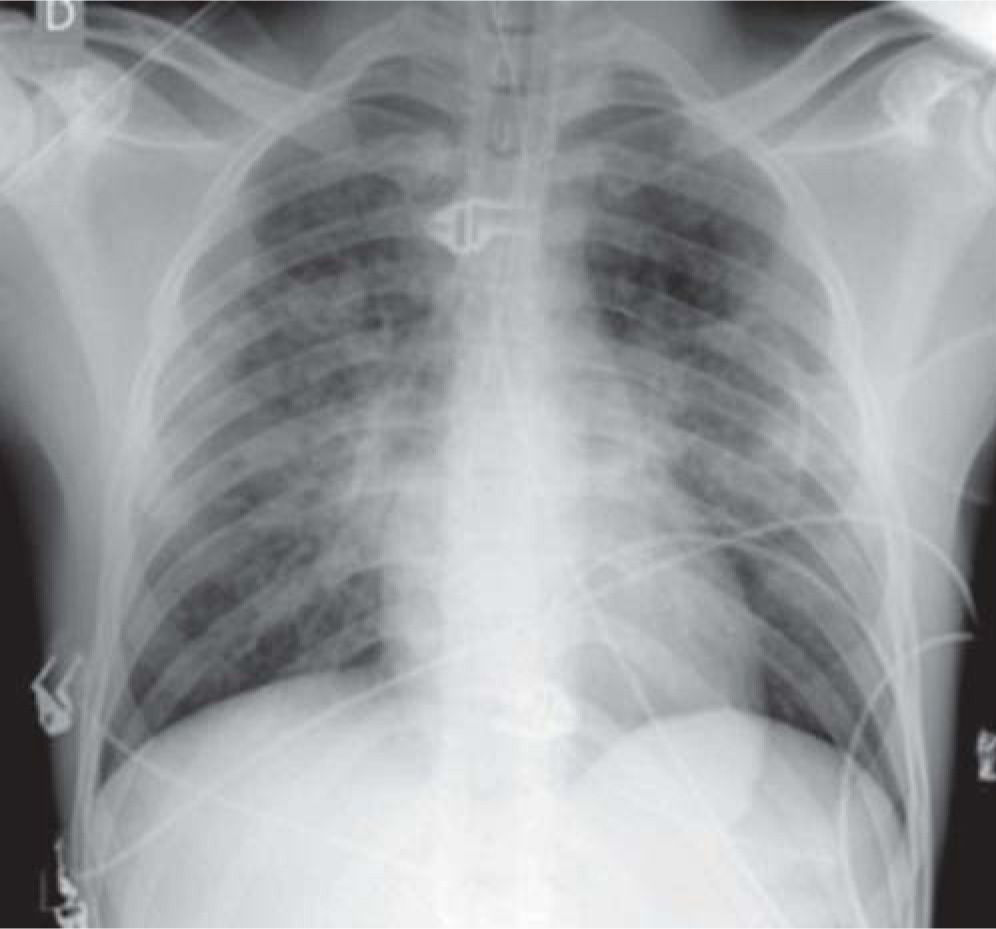
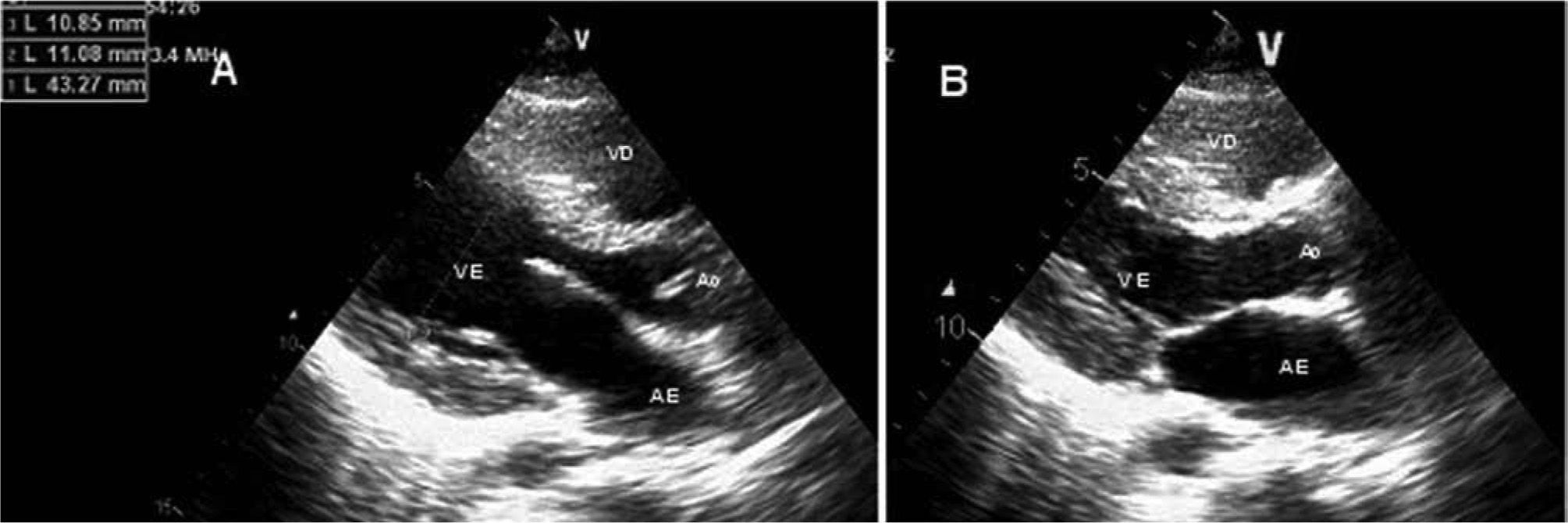
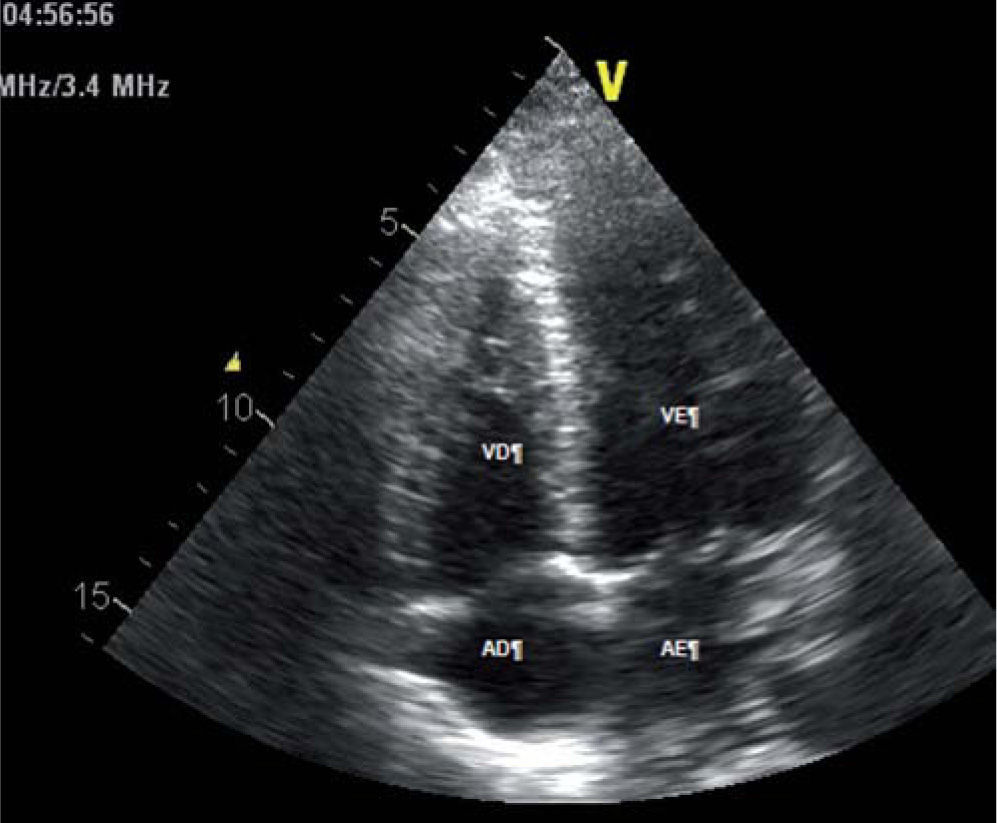
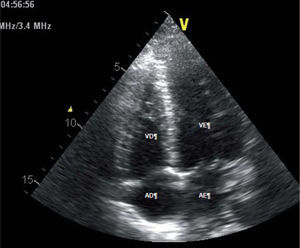
Case reportA 21-year-old man, black, a football player, was admitted via the emergency department with a clinical and laboratory diagnosis suggestive of acute appendicitis. There was no relevant family or personal history. Physical examination showed no abnormalities other than in the abdominal region. He underwent laparoscopic appendectomy under balanced general anesthesia, both of which were uneventful. The patient was extubated at the end of the procedure following reversal of neuromuscular blockade. Immediately after extubation, he developed a setting of respiratory distress, with abundant pink frothy sputum and significant arterial desaturation. Physical examination and chest X-ray revealed the presence of APE (Figure 1). After orotracheal reintubation and connection to a ventilator, the patient was transferred to our unit. Following treatment including high-flow oxygen therapy and administration of intravenous boluses of furosemide and isosorbide dinitrate, he showed rapid improvement and was extubated around four hours later (Figure 2). Other laboratory tests, together with electrocardiographic and echocardiographic assessment (Figures 3 and 4) excluded heart disease. There were no further complications.
APE in the immediate postoperative period can be cardiogenic, following a cardiac event during surgery, or non-cardiogenic, resulting from aspiration or laryngospasm. Post-extubation APE is an example of the latter; it is uncommon, occurring in 0.1% of patients undergoing surgery under general anesthesia3. The triggering factor, usually secondary to laryngospasm, is forceful inspiration against the closed glottis, which generates high negative intrathoracic pressures that can reach −100 cmH2O1-3.
The high incidence of this form of APE in young men, as shown by published series2-5, suggests that considerable muscular strength is required to generate marked negative intrathoracic pressure. As the negative pressure rises, it increases venous return to the right side of the heart, which in turn raises pulmonary venous pressure1. A transpulmonary gradient is thus created, with transudation of fluid into pulmonary alveoli and interstices, resulting in the clinical symptoms and signs of APE1,3. Mechanical stress also contributes to this situation, due to increased capillary permeability following disruption of alveolar epithelium and pulmonary capillary membranes1-3.
APE often resolves itself with support measures and oxygen therapy alone, but in some cases patients need to be reintubated and ventilated, which can be difficult and dangerous due to laryngospasm2-5. Even in these circumstances, prognosis is usually excellent, with rapid resolution and complete recovery2-5.
The case presented, of a young athlete who developed APE immediately after extubation and in whom the situation was rapidly and completely resolved despite requiring mechanical ventilation, is similar to those reported in the literature2,4,5. We have taken this opportunity to briefly review this uncommon but serious complication of upper airway obstruction.
Conflicts of interestThe authors have no conflicts of interest to declare.