Cardiology has not been seen as an attractive specialty, and women have avoided it for many years. Some surveys have been performed in other countries, but in Portugal, the situation is largely unknown.
MethodsAn online survey on perceptions of cardiology and professional preferences was sent to 1371 members of the Portuguese Society of Cardiology, of whom 18.2% completed the survey.
ResultsWe included 219 cardiologists or cardiology trainees, of whom 50.2% were female, with decreasing proportions from younger to older age groups, in which males still predominate. Women are less often married and more frequently childless, particularly those working in an invasive subspecialty, where they represent only 16% of all respondents working in these areas. Men's perception is that women do not choose these areas due to family reasons, radiation concerns and difficult working conditions, but from the female perspective, male dominance, lack of female role models and restricted access are the main barriers. Women consider it is difficult for them to obtain a leadership role, but men do not think the same (75.5% vs. 27.5%).
ConclusionIn Portugal, females predominate in younger age groups, suggesting a paradigm change. Women are less frequently married and more frequently childless, particularly women working in invasive subspecialties. Women consider that it is more difficult for them to obtain a leadership role. Moreover, the barriers reported by women are substantially different from men regarding the reasons for not choosing an invasive subspecialty.
A cardiologia não tem sido uma especialidade atrativa, que as mulheres têm habitualmente evitado. Alguns questionários foram realizados na Europa, mas em Portugal esta realidade é desconhecida.
MétodosFoi enviado um questionário online sobre a perceção da cardiologia e preferências profissionais a 1371 membros da Sociedade Portuguesa de Cardiologia, tendo 18,2% respondido.
ResultadosIncluíram-se no estudo 219 cardiologistas/internos de cardiologia, 50,2% mulheres, com aumentos progressivos da proporção de mulheres dos grupos etários mais jovens para os mais idosos, onde os homens ainda predominam. As mulheres são mais frequentemente solteiras e sem filhos, particularmente se trabalharem em áreas invasivas, onde elas representam apenas 16% dos respondedores que trabalham nessas áreas. A perceção masculina é de que as mulheres não escolhem as áreas invasivas por motivos familiares, preocupações com radiação e condições de trabalho difíceis. Contudo, a perspetiva feminina é de que as principais barreiras são a dominância masculina, ausência de role-models femininos e acesso restrito. As mulheres consideram também mais frequentemente que lhes é difícil chegar a lugares de liderança, não sendo essa a opinião global dos homens (75,5% versus 27,5%).
ConclusãoEm Portugal, as mulheres predominam nos grupos mais jovens, sugerindo uma mudança de paradigma. As mulheres são mais frequentemente solteiras e sem filhos, particularmente se trabalharem em áreas invasivas. Consideram que lhes é mais difícil atingir um lugar de liderança. As perspetivas femininas e masculinas relativas às barreiras colocadas às mulheres na escolha das áreas invasivas de subespecialização são substancialmente diferentes e até diametralmente opostas.
Cardiology has long been an unattractive medical area for young doctors, being seen as technically demanding, with long working hours and stressful situations. Moreover, women did not favor this medical specialty in the past and when they did, a noninvasive subspecialty was usually their choice.
In recent years, more women have been admitted to medical schools, and they now represent more than half of all physicians in the younger age groups working in medicine.1 Nevertheless, in cardiology women are still in the minority, despite substantial improvements in gender equity in recent years.2
In other countries, many motivations and barriers have been described by young trainees regarding the choice of cardiology as a specialty, particularly for invasive subspecialties. In a survey conducted in the US, the main perceptions of cardiology in young trainees were adverse job conditions, interference with family life, and a lack of diversity.3 Women and trainees who did not choose cardiology valued their work-life balance more highly and had more negative perceptions of cardiology than men or future cardiologists, who emphasized the professional advantages available in cardiology.3 Both professional development factors and perceptions of cardiology were strongly associated with the decision to pursue a career in cardiology in both genders.3
ObjectivesIn Portugal, this type of survey has never been conducted, and so the Women and Cardiology Task Force appointed by the 2021–2023 Board of the Portuguese Society of Cardiology (SPC) decided to analyze the situation in Portugal regarding professional choices in the field of cardiology, in both genders, but with a particular emphasis on women's career choices.
MethodsA structured questionnaire was developed by the Women and Cardiology Task Force of the SPC which included questions related to the respondents’ individual and family characteristics, as well as a detailed description of their professional, academic and research activities (Supplementary Figure). Some of the questions allowed multiple answers, to better characterize the reasons behind some professional choices.
This questionnaire was sent by e-mail to all members of the SPC. The purpose of the survey was explained to the participants, and informed consent was implicitly obtained through their anonymous and voluntary participation. The survey was made available through a Structured Query Language database specifically designed for the SPC and linked to the SPC members database. The study was conducted in accordance with the declaration of Helsinki.
Categorical data are presented as frequencies and percentages. A detailed statistical analysis was not the objective of the present survey; thus, no formal statistical comparisons were made.
ResultsThe questionnaire was sent to 1371 members of the Portuguese Society of Cardiology. A total of 250 individuals completed the survey, including 124 women (49.6%). The overall response rate was 18.2%. Of these, eight were pediatric cardiologists, five were cardiac surgeons, nine were from other allied medical specialties, eight were allied professionals and one did not reply to this question. Due to the small numbers of those specific professional branches and because there are different professional characteristics in these areas compared to cardiology, these individuals were excluded from the analysis. Therefore, we analyzed responses from 219 individuals (including 25 cardiology residents).
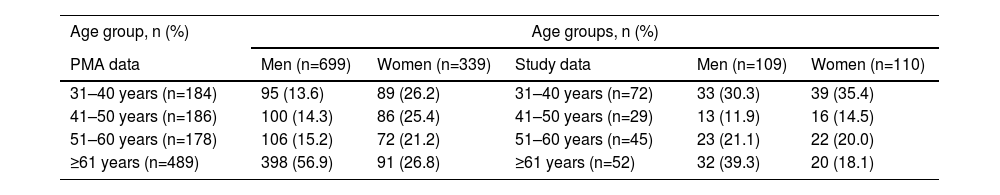
General characteristicsThe individuals included in the study were equally distributed by gender (50.2% female). Table 1 presents data from the Portuguese Medical Association (PMA) regarding medical doctors (not including trainees) in 2021, according to age group and gender.4 In our sample, there were more responders in the lowest age group (age 31–40 years) for both genders, compared to the national distribution of cardiologists, and fewer responders in the oldest age group. Regarding the male–female proportion according to age groups, the percentage of women was higher in our sample in the age groups below 50 years, and lower in the age group above 60 years, as also seen in the official national distribution.
Comparison of data from the Portuguese Medical Association and our study sample (only for cardiology specialists).
| Age group, n (%) | Age groups, n (%) | ||||
|---|---|---|---|---|---|
| PMA data | Men (n=699) | Women (n=339) | Study data | Men (n=109) | Women (n=110) |
| 31–40 years (n=184) | 95 (13.6) | 89 (26.2) | 31–40 years (n=72) | 33 (30.3) | 39 (35.4) |
| 41–50 years (n=186) | 100 (14.3) | 86 (25.4) | 41–50 years (n=29) | 13 (11.9) | 16 (14.5) |
| 51–60 years (n=178) | 106 (15.2) | 72 (21.2) | 51–60 years (n=45) | 23 (21.1) | 22 (20.0) |
| ≥61 years (n=489) | 398 (56.9) | 91 (26.8) | ≥61 years (n=52) | 32 (39.3) | 20 (18.1) |
PMA: Portuguese Medical Association.
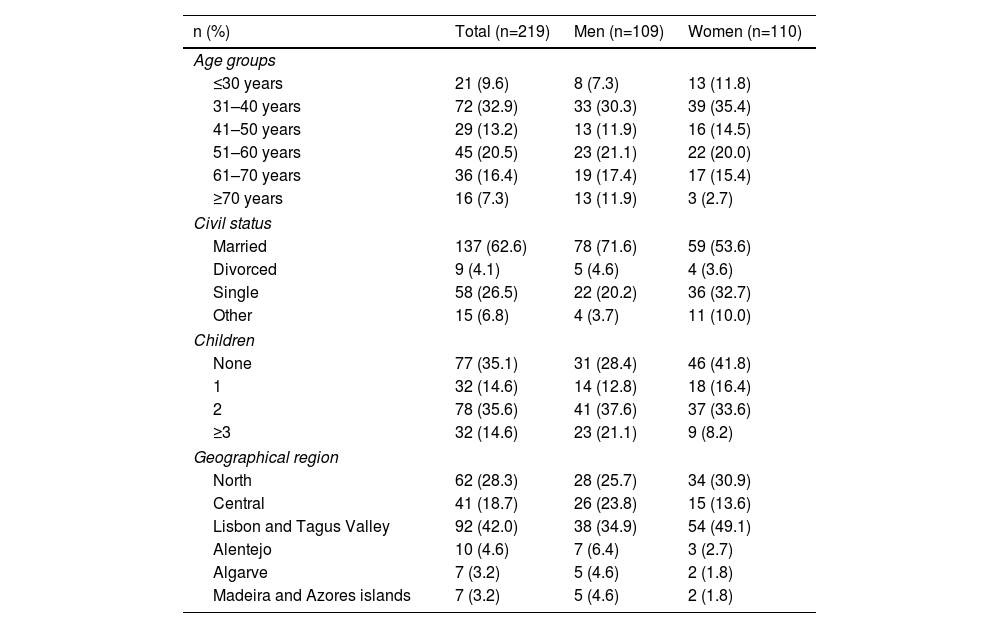
Table 2 shows a detailed description of the participants’ general characteristics. Women predominate in the age groups below 50 years (55.7%), while men predominate in those aged over 50 years (56.7%). Regarding marital status, in general, there are more married men than women and more single women than men. Moreover, men have more children and women are more frequently childless. Regarding geographical distribution, in our sample both men and women work predominantly in the Lisbon and Tagus Valley region, as well as in the North region, followed by the Central region, with fewer respondents from other regions of the country. In the Lisbon region and the North, women predominate, but in all other geographical areas there were more male responders.
General characteristics of the study population.
| n (%) | Total (n=219) | Men (n=109) | Women (n=110) |
|---|---|---|---|
| Age groups | |||
| ≤30 years | 21 (9.6) | 8 (7.3) | 13 (11.8) |
| 31–40 years | 72 (32.9) | 33 (30.3) | 39 (35.4) |
| 41–50 years | 29 (13.2) | 13 (11.9) | 16 (14.5) |
| 51–60 years | 45 (20.5) | 23 (21.1) | 22 (20.0) |
| 61–70 years | 36 (16.4) | 19 (17.4) | 17 (15.4) |
| ≥70 years | 16 (7.3) | 13 (11.9) | 3 (2.7) |
| Civil status | |||
| Married | 137 (62.6) | 78 (71.6) | 59 (53.6) |
| Divorced | 9 (4.1) | 5 (4.6) | 4 (3.6) |
| Single | 58 (26.5) | 22 (20.2) | 36 (32.7) |
| Other | 15 (6.8) | 4 (3.7) | 11 (10.0) |
| Children | |||
| None | 77 (35.1) | 31 (28.4) | 46 (41.8) |
| 1 | 32 (14.6) | 14 (12.8) | 18 (16.4) |
| 2 | 78 (35.6) | 41 (37.6) | 37 (33.6) |
| ≥3 | 32 (14.6) | 23 (21.1) | 9 (8.2) |
| Geographical region | |||
| North | 62 (28.3) | 28 (25.7) | 34 (30.9) |
| Central | 41 (18.7) | 26 (23.8) | 15 (13.6) |
| Lisbon and Tagus Valley | 92 (42.0) | 38 (34.9) | 54 (49.1) |
| Alentejo | 10 (4.6) | 7 (6.4) | 3 (2.7) |
| Algarve | 7 (3.2) | 5 (4.6) | 2 (1.8) |
| Madeira and Azores islands | 7 (3.2) | 5 (4.6) | 2 (1.8) |
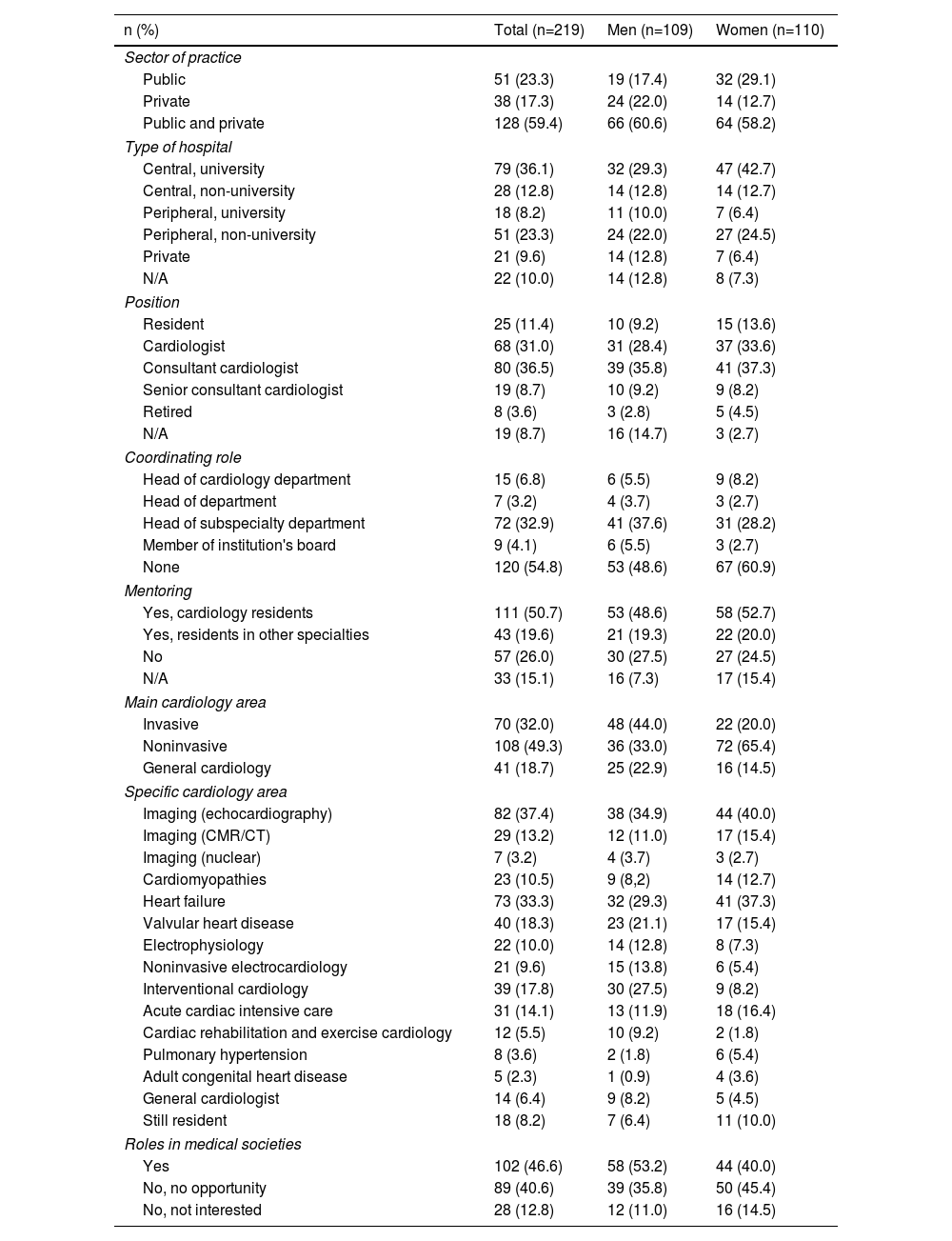
Table 3 shows the characterization of professional practice. There are more men working exclusively in private practice and more women exclusively in the public sector, and the proportion is similar for those who work in both private and public sectors. Most women work in central university hospitals (43%), and one-fourth work in peripheral non-university hospitals. For men, the distribution is more even, with a slight predominance in central university hospitals and peripheral non-university hospitals. In our sample, there are more women working as residents, and thereafter there is a slight and progressive decrease for other positions, with similar proportions beyond the level of consultant cardiologist. Interestingly, there are more women who are head of a cardiology department, but not in other roles. In fact, more women than men have no coordinating role. Regarding mentoring activities, the results are similar for both genders.
Characteristics of professional practice.
| n (%) | Total (n=219) | Men (n=109) | Women (n=110) |
|---|---|---|---|
| Sector of practice | |||
| Public | 51 (23.3) | 19 (17.4) | 32 (29.1) |
| Private | 38 (17.3) | 24 (22.0) | 14 (12.7) |
| Public and private | 128 (59.4) | 66 (60.6) | 64 (58.2) |
| Type of hospital | |||
| Central, university | 79 (36.1) | 32 (29.3) | 47 (42.7) |
| Central, non-university | 28 (12.8) | 14 (12.8) | 14 (12.7) |
| Peripheral, university | 18 (8.2) | 11 (10.0) | 7 (6.4) |
| Peripheral, non-university | 51 (23.3) | 24 (22.0) | 27 (24.5) |
| Private | 21 (9.6) | 14 (12.8) | 7 (6.4) |
| N/A | 22 (10.0) | 14 (12.8) | 8 (7.3) |
| Position | |||
| Resident | 25 (11.4) | 10 (9.2) | 15 (13.6) |
| Cardiologist | 68 (31.0) | 31 (28.4) | 37 (33.6) |
| Consultant cardiologist | 80 (36.5) | 39 (35.8) | 41 (37.3) |
| Senior consultant cardiologist | 19 (8.7) | 10 (9.2) | 9 (8.2) |
| Retired | 8 (3.6) | 3 (2.8) | 5 (4.5) |
| N/A | 19 (8.7) | 16 (14.7) | 3 (2.7) |
| Coordinating role | |||
| Head of cardiology department | 15 (6.8) | 6 (5.5) | 9 (8.2) |
| Head of department | 7 (3.2) | 4 (3.7) | 3 (2.7) |
| Head of subspecialty department | 72 (32.9) | 41 (37.6) | 31 (28.2) |
| Member of institution's board | 9 (4.1) | 6 (5.5) | 3 (2.7) |
| None | 120 (54.8) | 53 (48.6) | 67 (60.9) |
| Mentoring | |||
| Yes, cardiology residents | 111 (50.7) | 53 (48.6) | 58 (52.7) |
| Yes, residents in other specialties | 43 (19.6) | 21 (19.3) | 22 (20.0) |
| No | 57 (26.0) | 30 (27.5) | 27 (24.5) |
| N/A | 33 (15.1) | 16 (7.3) | 17 (15.4) |
| Main cardiology area | |||
| Invasive | 70 (32.0) | 48 (44.0) | 22 (20.0) |
| Noninvasive | 108 (49.3) | 36 (33.0) | 72 (65.4) |
| General cardiology | 41 (18.7) | 25 (22.9) | 16 (14.5) |
| Specific cardiology area | |||
| Imaging (echocardiography) | 82 (37.4) | 38 (34.9) | 44 (40.0) |
| Imaging (CMR/CT) | 29 (13.2) | 12 (11.0) | 17 (15.4) |
| Imaging (nuclear) | 7 (3.2) | 4 (3.7) | 3 (2.7) |
| Cardiomyopathies | 23 (10.5) | 9 (8,2) | 14 (12.7) |
| Heart failure | 73 (33.3) | 32 (29.3) | 41 (37.3) |
| Valvular heart disease | 40 (18.3) | 23 (21.1) | 17 (15.4) |
| Electrophysiology | 22 (10.0) | 14 (12.8) | 8 (7.3) |
| Noninvasive electrocardiology | 21 (9.6) | 15 (13.8) | 6 (5.4) |
| Interventional cardiology | 39 (17.8) | 30 (27.5) | 9 (8.2) |
| Acute cardiac intensive care | 31 (14.1) | 13 (11.9) | 18 (16.4) |
| Cardiac rehabilitation and exercise cardiology | 12 (5.5) | 10 (9.2) | 2 (1.8) |
| Pulmonary hypertension | 8 (3.6) | 2 (1.8) | 6 (5.4) |
| Adult congenital heart disease | 5 (2.3) | 1 (0.9) | 4 (3.6) |
| General cardiologist | 14 (6.4) | 9 (8.2) | 5 (4.5) |
| Still resident | 18 (8.2) | 7 (6.4) | 11 (10.0) |
| Roles in medical societies | |||
| Yes | 102 (46.6) | 58 (53.2) | 44 (40.0) |
| No, no opportunity | 89 (40.6) | 39 (35.8) | 50 (45.4) |
| No, not interested | 28 (12.8) | 12 (11.0) | 16 (14.5) |
CMR: cardiac magnetic resonance; CT: computed tomography; N/A: not applicable.
Invasive subspecialization is more frequent in the male group, with women preferring noninvasive subspecialties. We also found that most participants have more than one activity in cardiology, with only 66 participants (30.1%) working in a single specialist area, mostly in interventional cardiology or electrophysiology, and slightly more frequently in men (34.3% vs. 30.5%). Men predominate in invasive areas, such as electrophysiology and interventional cardiology, and in other areas such as cardiac rehabilitation, sports and exercise cardiology, and noninvasive electrocardiology. Interestingly, the male/female distribution for noninvasive imaging is similar, and women predominate only in the subspecialties of heart failure, cardiomyopathies, acute cardiac intensive care, pulmonary hypertension and adult congenital heart disease.
More men have a present or past role in a medical society and more women claim that they never had an opportunity to do so. However, the proportions of those who are not interested in having roles in medical societies are similar.
Characterization of women in invasive subspecialtiesData from the PMA show that there are 93 subspecialists in interventional cardiology in Portugal, but only 12.9% of them are women.4 In electrophysiology, there are 32 subspecialists, of whom 25% are women.4 In total, 16% of those working officially in these invasive subspecialties are women. Looking at our own data, a total of 70 respondents work in an invasive area, not very different from what is reported by the PMA. Of these, 22 (31%) are women, suggesting that a greater number of women working in invasive areas responded to this survey, even considering that some responders might not be yet subspecialists in this area according to the PMA.
In a head-to-head comparison between women and men working in invasive areas, women are less frequently married (40.9% vs. 62.5%) and are more frequently childless (59.1% vs. 35.3%). If married, in both genders, they are mostly married to another medical doctor (67–70%), followed by a non-health professional (17–22%), and finally to another health professional (11–13%).
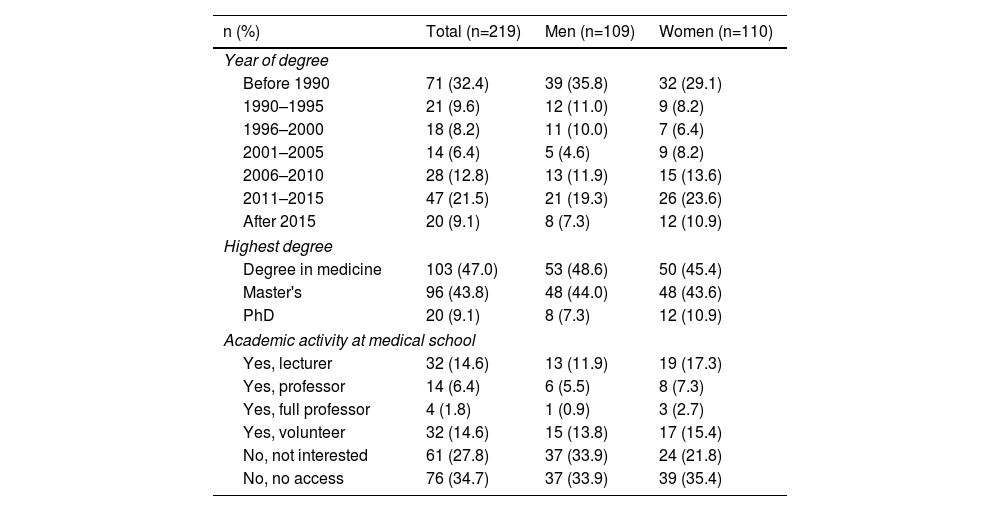
Academic and research activitiesAlmost 45% of respondents have a master's degree (similar in both genders). However, only 9% have a PhD, and interestingly, more of these are women (Table 4). Regarding academic activities, there are slightly more women participating in all types of activities, with similar access. Moreover, more men have no interest in participating in academic activities.
Academic characteristics.
| n (%) | Total (n=219) | Men (n=109) | Women (n=110) |
|---|---|---|---|
| Year of degree | |||
| Before 1990 | 71 (32.4) | 39 (35.8) | 32 (29.1) |
| 1990–1995 | 21 (9.6) | 12 (11.0) | 9 (8.2) |
| 1996–2000 | 18 (8.2) | 11 (10.0) | 7 (6.4) |
| 2001–2005 | 14 (6.4) | 5 (4.6) | 9 (8.2) |
| 2006–2010 | 28 (12.8) | 13 (11.9) | 15 (13.6) |
| 2011–2015 | 47 (21.5) | 21 (19.3) | 26 (23.6) |
| After 2015 | 20 (9.1) | 8 (7.3) | 12 (10.9) |
| Highest degree | |||
| Degree in medicine | 103 (47.0) | 53 (48.6) | 50 (45.4) |
| Master's | 96 (43.8) | 48 (44.0) | 48 (43.6) |
| PhD | 20 (9.1) | 8 (7.3) | 12 (10.9) |
| Academic activity at medical school | |||
| Yes, lecturer | 32 (14.6) | 13 (11.9) | 19 (17.3) |
| Yes, professor | 14 (6.4) | 6 (5.5) | 8 (7.3) |
| Yes, full professor | 4 (1.8) | 1 (0.9) | 3 (2.7) |
| Yes, volunteer | 32 (14.6) | 15 (13.8) | 17 (15.4) |
| No, not interested | 61 (27.8) | 37 (33.9) | 24 (21.8) |
| No, no access | 76 (34.7) | 37 (33.9) | 39 (35.4) |
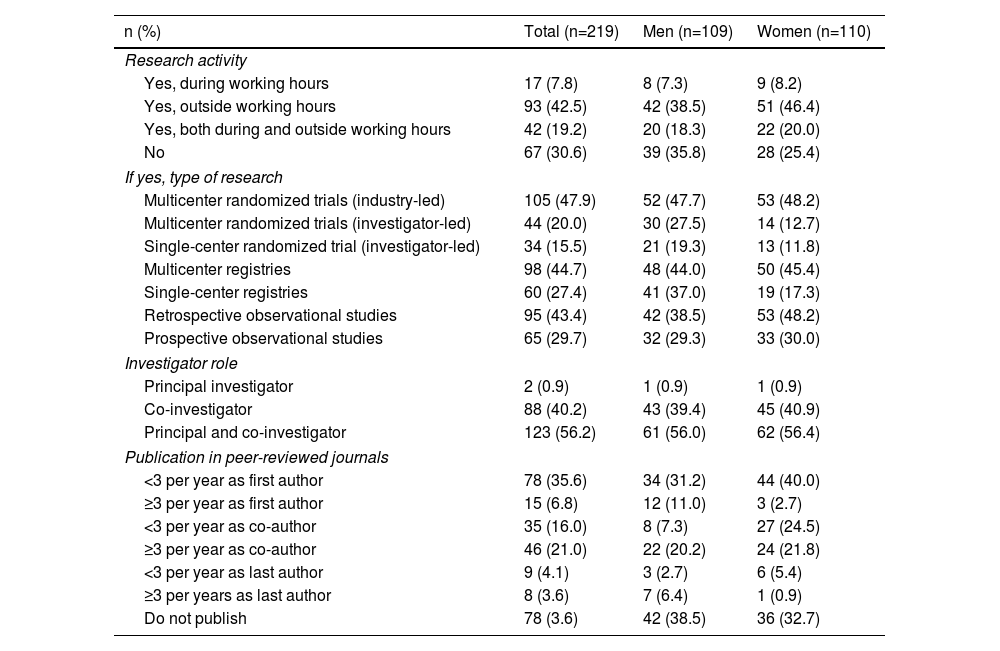
Regarding research, almost 70% have an active role, mostly performed outside normal working hours, with only 8% reporting that they carry out research during their official working hours (Table 5). Nevertheless, more men than women (36% vs. 25%) do not carry out any research. Regarding the role of investigator, the male/female ratio is similar for all roles. Furthermore, men are more often involved in investigator-led research, in both single-center and multicenter randomized trials, and single-center registries, and women participate more in retrospective observational studies. Men publish more frequently (≥3 publications in peer-reviewed journals per year) compared to women as first author and similarly as co-author. This difference was also found in the age groups below 40 years, with 42.3% of women and 65.8% of men publishing frequently as first authors. Moreover, in young individuals, 27% of women but only 17% of men do not publish at all. Moreover, men are more often frequent publishers as last author.
Research activities.
| n (%) | Total (n=219) | Men (n=109) | Women (n=110) |
|---|---|---|---|
| Research activity | |||
| Yes, during working hours | 17 (7.8) | 8 (7.3) | 9 (8.2) |
| Yes, outside working hours | 93 (42.5) | 42 (38.5) | 51 (46.4) |
| Yes, both during and outside working hours | 42 (19.2) | 20 (18.3) | 22 (20.0) |
| No | 67 (30.6) | 39 (35.8) | 28 (25.4) |
| If yes, type of research | |||
| Multicenter randomized trials (industry-led) | 105 (47.9) | 52 (47.7) | 53 (48.2) |
| Multicenter randomized trials (investigator-led) | 44 (20.0) | 30 (27.5) | 14 (12.7) |
| Single-center randomized trial (investigator-led) | 34 (15.5) | 21 (19.3) | 13 (11.8) |
| Multicenter registries | 98 (44.7) | 48 (44.0) | 50 (45.4) |
| Single-center registries | 60 (27.4) | 41 (37.0) | 19 (17.3) |
| Retrospective observational studies | 95 (43.4) | 42 (38.5) | 53 (48.2) |
| Prospective observational studies | 65 (29.7) | 32 (29.3) | 33 (30.0) |
| Investigator role | |||
| Principal investigator | 2 (0.9) | 1 (0.9) | 1 (0.9) |
| Co-investigator | 88 (40.2) | 43 (39.4) | 45 (40.9) |
| Principal and co-investigator | 123 (56.2) | 61 (56.0) | 62 (56.4) |
| Publication in peer-reviewed journals | |||
| <3 per year as first author | 78 (35.6) | 34 (31.2) | 44 (40.0) |
| ≥3 per year as first author | 15 (6.8) | 12 (11.0) | 3 (2.7) |
| <3 per year as co-author | 35 (16.0) | 8 (7.3) | 27 (24.5) |
| ≥3 per year as co-author | 46 (21.0) | 22 (20.2) | 24 (21.8) |
| <3 per year as last author | 9 (4.1) | 3 (2.7) | 6 (5.4) |
| ≥3 per years as last author | 8 (3.6) | 7 (6.4) | 1 (0.9) |
| Do not publish | 78 (3.6) | 42 (38.5) | 36 (32.7) |
In general, a majority of responders (51.0%) consider that in Portugal, women have more difficulties in achieving leadership roles. Interestingly, this perception was much stronger in women than in men (75.5% vs. 27.5%). On this question 5.5% gave no formal opinion.
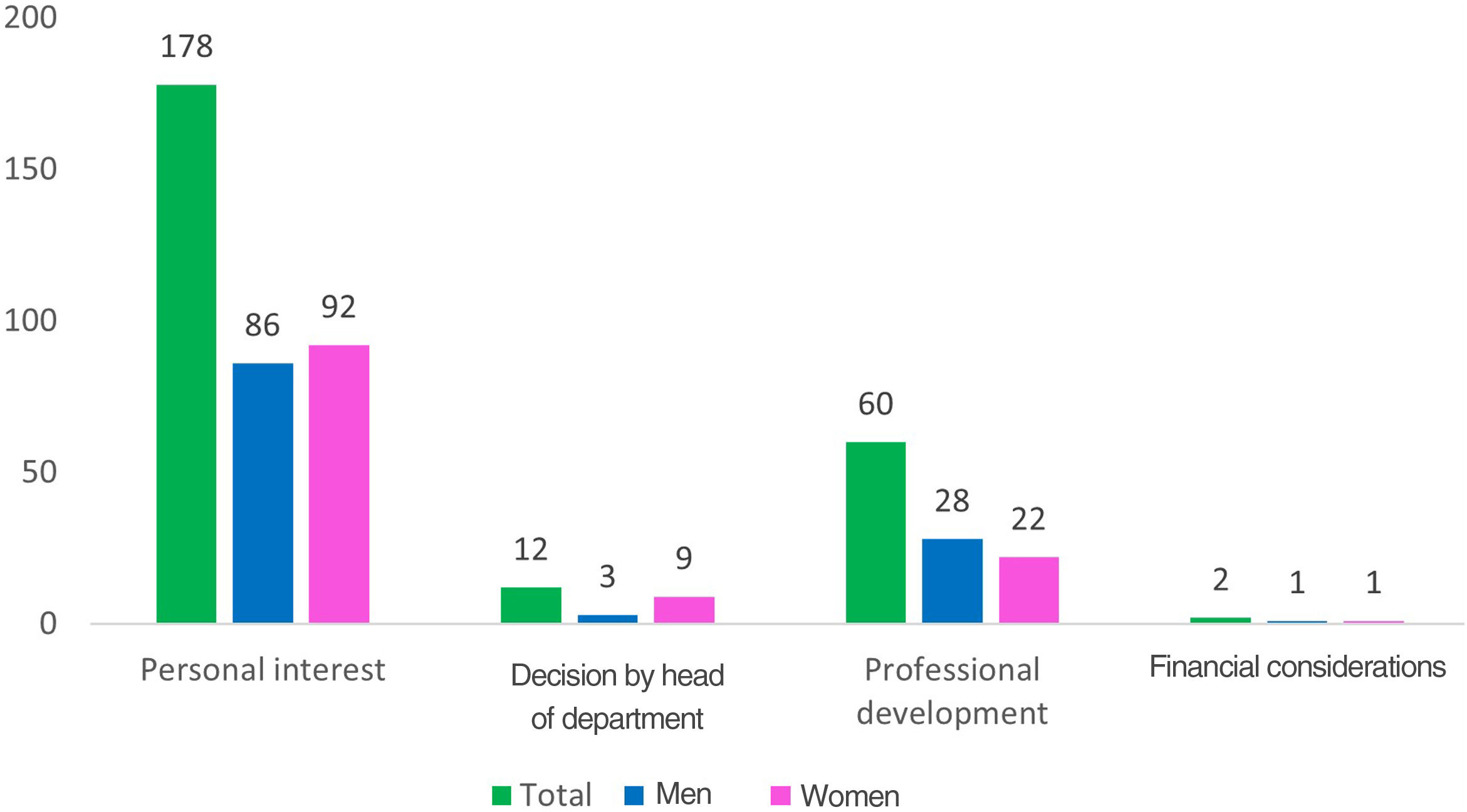
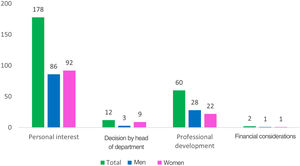
When replying to the question regarding the motive for choosing a particular area of specialization, most respondents considered that it was because of a personal interest in the topic, followed by the need for professional development, while in a minority, mostly women, it was due to a decision by the head of the cardiology department (Figure 1). Financial considerations were not a reason for choosing a specific subspecialty.
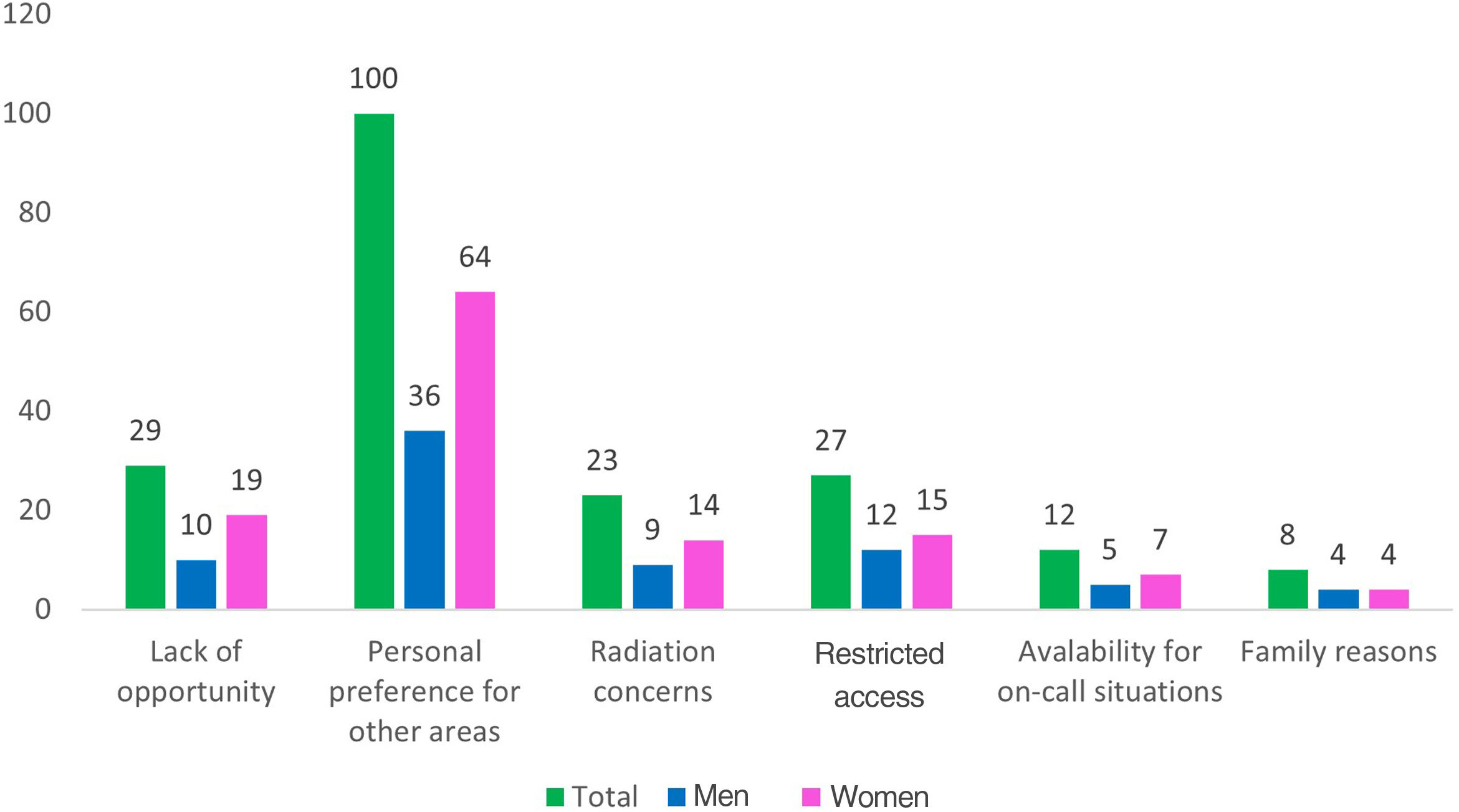
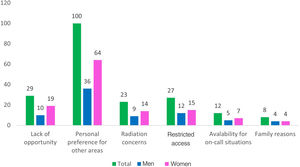
The most frequent reason for not choosing an invasive subspecialty or one with radiation exposure was personal interest in other areas (similar in both genders), but 15–19% also highlight lack of opportunity, restricted access and radiation concerns, particularly in women (Figure 2). Availability for on-call work and family reasons were also cited, but less frequently and at similar rates for men and women.
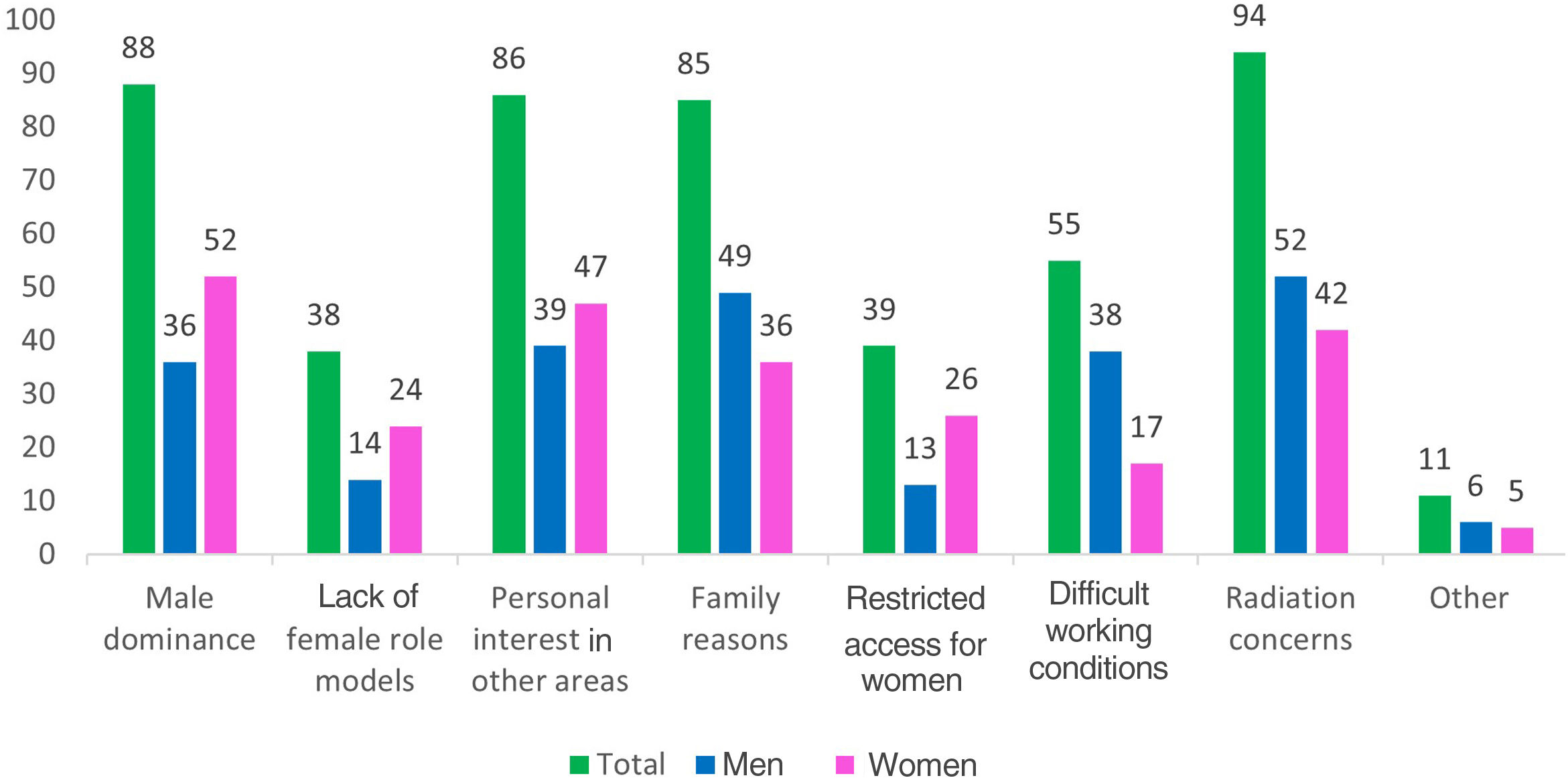
Regarding the question why women less often choose invasive subspecialties, the general perception is that it is mostly related to radiation concerns, male dominance, personal interest in other areas, and family reasons (Figure 3). However, the main reasons perceived by women are male dominance, the lack of female role models and restricted access. By contrast, men's perception is that radiation concerns, family reasons and difficult working conditions are the main reasons.
DiscussionFor many years, cardiology has been perceived as a highly demanding specialty, particularly for women. Previous surveys have been carried out, mainly in the US, one of which was conducted in internal medicine trainees in 2009 to understand their preferences for professional development and perceptions of cardiology and the influence of those perceptions and preferences on the trainees’ career choices.3 A total of 1123 trainees in residency programs completed the survey, 55.7% of them men. The investigators concluded that factors determining professional career development preferences were stable hours, family and female friendliness, the availability of positive role models, financial benefits, professional challenges, patient focus, and the opportunity to have a stimulating career. Contrariwise, the main perceptions about cardiology were adverse job conditions, interference with family life, and a lack of diversity. Interestingly, women and trainees who did not choose cardiology valued work-life balance more highly and had more negative perceptions of cardiology than men or future cardiologists, who emphasized the professional advantages available in cardiology. It was also clear in this survey that prospects of professional development and adverse perceptions of cardiology were strongly associated with the decision to pursue or avoid a career in cardiology in both genders. The same survey was applied 10 years later; both male and female residents placed a high value on support for optimal work-life balance, which increased over the ensuing decade, particularly in male residents.5 Furthermore, residents in the later survey were more likely than their predecessors to agree with negative perceptions of cardiology. Therefore, in the US there is currently a change in preferences in both men and women, which should call attention to the need to improve the culture of cardiology in order to make this specialty a more attractive career choice for all. In Portugal, and especially among young doctors, job satisfaction, quality of life and work-family balance are also important factors taken into consideration when making professional choices.6 It is thus not surprising that cardiology is not currently among the top choices of medical specialties in Portugal.
Although the gender imbalance is beginning to shift in both the US and Europe, with women accounting for almost 50% of medical school graduates and medical doctors, this is not the case when considering gender distribution in some specialties, particularly in cardiology.1,4,7–9 In the US, 42.6% of internal medicine resident physicians are women, but in cardiology, women account for 21.5% and only 12.6% of practicing cardiologists are women.7 Moreover, regarding cardiology subspecialties, in some areas the balance clearly shifts to male dominance. Interventional cardiology has traditionally been a male-only field, and this picture is consistent around the globe: in the US, only 5.9% of board-certified interventional cardiologists are women, and in Italy, just 12.5%.7–9 In some European countries, there has been some progress. Data from the European Society of Cardiology 2019 Atlas show that in Europe, there are an average of 81 cardiologists per 1000000 population (89 cardiologists in Portugal), but only one-third (28%) are women, with significant under-representation of females in Kosovo, the UK and Ireland, where women comprise <15% of cardiologists, but in other countries >70% of cardiologists are women, such as Latvia, Lithuania, Moldova and Armenia.10
There have also been changes regarding professional preferences among cardiologists and cardiology residents. A study from the American College of Cardiology compared serial survey results obtained in the previous 20 years.11 In the last survey, 21% of members completed the questionnaire, 58% men, and 13% fellows-in-training. Compared with 10 and 20 years before, the cardiology workforce is aging, and most cardiologists no longer report working in a private practice setting. Women continue to be more likely to practice in academic centers and have a noninvasive subspecialty. Men were more likely than previously to indicate that family responsibilities negatively influenced their careers, whereas women remained less likely to marry or have children. They both reported similarly high levels of career satisfaction, with women reporting higher satisfaction currently. Nevertheless, two-thirds of women continue to experience discrimination, nearly three times the rate in men. This continues to be an issue reported by a clear majority of female cardiologists. Overall, personal life choices continue to differ substantially for men and women in cardiology, although the differences have diminished over time.
In Europe, data regarding professional preferences and women in cardiology are scarce. In Spain, in the last decade women have represented 68% of cardiology residents and 40% of all practicing cardiologists.12 In 2021, according to data from the PMA, Portuguese women accounted for 33% of all practicing cardiologists, slightly higher than the average in Europe, but lower than in Spain, and still with an asymmetric distribution by age group: 24% of female cardiologists are over the age of 50, rising to 47% in those under 50 years old.4 These gender differences are often attributed to women's unwillingness to go into medical specialties that are assumed to be more demanding and interfere more with family life, and to invest in an academic career, which is less stable than a clinical career. Furthermore, in Spain, women represent only 19% of department heads and only 11% of section heads; in Portugal these numbers are even worse. Moreover, in the UK, significant salary inequities are reported, with men receiving 17% more.13 Wage disparities are often explained as a result of women working part-time or limited hours or choosing lower-paying specialties to allow for more time off to raise a family. However, even after accounting for specialty, hours worked and other measures of productivity and achievement, women still earn less than their male counterparts. In addition, women are under-represented in medical societies.14 Of the ESC membership, in 2019 female cardiologists accounted for around 33% in the group aged 40–50 years, and even fewer for those aged >55 years (16–28%). Moreover, although there have been more female cardiologists on the ESC board and committees over the last decade, in 2019 they were still under-represented, with 31% and 28%, respectively. The same is also apparent when considering women on the editorial boards of major US and European cardiology journals, as well as in academic medicine. In the UK, women account for 26.3% of clinical academics, 42.3% of lecturers and only 15.6% of full professors.15
Our survey encompasses all subspecialties, including fellows-in-training, and all age groups, and women and men are equally represented, which enables the survey to present a balanced view of gender differences. It also has a geographical distribution that follows the national distribution of cardiologists. In agreement with data from the PMA, women predominate in younger age groups, unlike in older groups. Similarly to US data, women are less likely to be married and are more often childless. Similar proportions of men and women work simultaneously in the public and private sectors. This shows that women are not hindered from working in both types of practice, but men are more likely to work exclusively in the private sector.
In our survey, women predominate in lower hierarchical positions, but not in leadership roles. However, the difference in the higher roles is not very striking, which might be one of the biases caused by the survey's higher response rate from women. Nevertheless, more women have no coordinating role. Moreover, both genders have mentoring activities, suggesting that for this activity, gender does not seem to be an issue. Regarding activities in medical societies, men are more frequently involved, while more women than men claim that they have not had the opportunity to do so. Women therefore seem to have some difficulty in gaining access to such activity.
Some European surveys have been conducted in the areas of interventional cardiology and electrophysiology, the subspecialties with the lowest female representation and in which the gender gap is most marked. Very few women become interventional cardiologists, even though a substantial proportion of younger cardiologists and most medical students are now women. In Europe women are still under-represented in this field, accounting for as few as 5.7% of physicians in interventional cardiology in countries such as the UK.16 The European Association of Percutaneous Cardiovascular Interventions (EAPCI) conducted a worldwide survey of health professionals with an interest in interventional cardiology, aiming to better understand the motivations and barriers for women in selecting interventional cardiology as a career path.17 In this survey, 60.7% of all respondents were women, who were less frequently married than men (57.0% vs. 79.8%) and more frequently childless (46.6% vs. 20.5%). In Portugal, there are a few more women working in interventional cardiology (12.9%) according to data from the PMA. However, these results are in line with the EAPCI survey.
In the EAPCI survey, the most frequent reason for choosing interventional cardiology was passion, while arguments against were lack of opportunity, radiation concerns and preference.17 Many reasons are reported for women choosing not to enter the field of interventional cardiology, but one of the main factors is probably that training often coincides with childbearing age and interferes with family planning.16 In addition, unpredictable schedules and long training hours make related choices complex. Finally, radiation exposure during pregnancy introduces an added risk. From men's perspective, the main reason for women not choosing this subspecialty is on-calls and long working hours.17 In our survey, both genders gave the main reason for not choosing an invasive subspecialty as a personal interest in other areas. However, lack of opportunity, radiation concerns and restricted access are also relevant, particularly from women's perspective. When asked specifically why women usually do not choose an invasive subspecialty, different answers were obtained. For women, the main reasons perceived are male dominance, the lack of female role models and restricted access. By contrast, men's perception is that radiation concerns, family reasons and difficult working conditions are the main reasons. Another interesting result is that in our survey, more women than men are working in cardiac intensive care, which is currently a very hard and demanding subspecialty, showing that this factor is not an obstacle for women, and that men's perception is incorrect.
Surprisingly, women do not consider that radiation concerns are a major barrier for them to be working in areas with radiation exposure. Nevertheless, in most surveys, the radiation issue is usually mentioned as an important barrier to women's participation and pursuing a career in interventional cardiology or cardiac electrophysiology, and this may also lead to a prolonged interruption in their career for those that choose it.18 Accordingly, EAPCI, the European Heart Rhythm Association, the European Association of Cardiovascular Imaging, the ESC Regulatory Affairs Committee and Women as One recently published a joint statement on radiation protection for healthcare professionals working in catheterization laboratories during pregnancy.19 This document puts forward important proposals for improving workplace safety and encouraging gender equity.
In general, a high proportion of participants do some form of research. However, nearly 30% (more frequently men) do not participate in research. Importantly, this activity is usually performed outside normal working hours, which is an additional difficulty. But in this survey, there appears to be gender equity regarding research. Nonetheless, when we look at publications, men publish more frequently, both as principal author and as co-author. This is also seen in younger age groups. In a previous publication, it was shown that in Portugal women accounted for around 50% of authorship in original articles published in the Portuguese Journal of Cardiology.2 However, current data do not corroborate these conclusions. The probable explanation for this contradictory finding is that currently, residents are under more pressure to publish in higher-impact journals, which have a gender equity problem, as previously highlighted.20 It is also important to stress that men publish as a senior author more often than women, which is also not surprising, due to the national gender gap in heads of department and sections.
Our survey complements information provided by a previous online survey sent to the Portuguese cardiology community, to better understand how they feel about their work.21 It showed that in general, they work for more than 45 hours per week, particularly when working in both the public and private sector, with 74% of those in the public sector wishing to reduce their weekly working hours. Importantly, around eight hours a week were spent in administrative work in the public sector. Overall, only 47% reported satisfaction with sleep quality, and anxiety and depression were reported in around 25% of respondents. In general, less than five hours per week were spent on exercise, hobbies and cultural activities; it should also be noted that around one-third do not take any exercise or have a hobby, and half responded that they had no time for cultural activities. This shows important quality of life issues. In general, they had low levels of job satisfaction, in both intrinsic (career, income, work content and decision-making autonomy) and extrinsic domains (working hours, organizational resources and support, work-life balance), and high levels of emotional exhaustion (similar between genders, but more significant in the public sector). Job satisfaction had a positive impact on reducing burnout, highlighting the importance of work-related factors in reducing occupational health threats. Nevertheless, 90% still moderately or highly recommend this specialty. Of note, in this survey, 52% of the respondents were female, and therefore women were well represented.
Some concrete and actionable solutions at individual and institutional levels have been suggested to attract women and encourage them to enter cardiology.14 At an individual level, women should recognize the importance of participating in academic and clinical decision-making processes. At an institutional level, adjustments should be made to support career flexibility and work-family balance, as well as equal pay and access to management boards. In addition, female mentorship should be improved, particularly by increasing the number of female role models. Participation in national and international networks, leadership research, collaboration in clinical trials, sponsorship opportunities, and membership of management boards, journal editorial boards and scientific advisory boards (based on merit) are additional keys to success.
LimitationsUnlike the situation in Portugal as a whole, where only around one-third of cardiologists are women, in our survey 50% of respondents were women. Therefore, the results may be an over-representation of the opinions and practices of women. Although we tried to avoid linking the survey to the Women and Cardiology Task Force in the invitation sent for participation (only the SPC was mentioned), it is generally observed that in other international surveys conducted to better understand the barriers and motivations for choosing a specific subspecialty, women usually account for around 50% of respondents. However, the male/female distribution according to age groups in the survey is fairly similar to that reported by the PMA, and all age groups are adequately represented. Moreover, that good representation of women allows us to make appropriate comparisons regarding gender-based opinions on professional preferences.
Another limitation is the relatively small sample of participants. Nevertheless, in other similar surveys, the response rate is usually around 20%, similar to that seen in our survey.
ConclusionsIn cardiology in Portugal, women predominate in younger age groups, but not in older ones. Women are less frequently married and more frequently childless, particularly when working in invasive subspecialties, in which women are still in the minority. It is also noteworthy that men think that the reasons for women not choosing an invasive subspecialty are the difficult working conditions, family issues and radiation concerns. However, from a female perspective, the reasons are related to male dominance, lack of role models and restricted access. In fact, there are more women working in acute cardiac care, which is also a very demanding subspecialty. Men are less interested in academic activities, and in general, they perform research less frequently. However, they publish more often as first as well as a senior author. The fact that in real life there are more men as head of department or section is one of the main reasons for this.
FundingNone to declare.
Conflicts of interestThe authors have no conflicts of interest to declare.