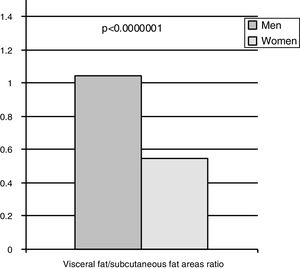
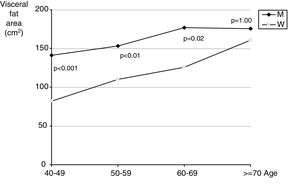
It is well known that the prevalence of cardiovascular disease is greater in men than in women. Sex hormones are believed to be involved in the relative protection from cardiovascular events in premenopausal women. After menopause the prevalence of cardiovascular disease in women increases gradually to the levels seen in men. These differences may be explained to a considerable extent by differences in body fat distribution and the consequences of visceral fat accumulation. There are marked anatomical differences between human males and females, attributable to body fat distribution that is unique to our species.1 We studied the relationship between the pattern of body fat distribution, quantified by a direct method (computed tomography [CT]) and the risk and risk factors for coronary heart disease, including, among other parameters, blood pressure, lipid levels, glucose homeostasis, smoking, exercise levels and family history of coronary heart disease.2 In addition, we compared the distribution of body fat between cases of acute myocardial infarction and community controls in a case-control study.2 In this direct measurement, men had more visceral fat (p<0.00001) and less subcutaneous fat (p<0.0001) than women, with no differences in total fat (Figure 1).2 The amount of visceral adipose tissue is more than twice as high in men as in premenopausal women.2,3 Visceral fat deposition increases with age in men and particularly in postmenopausal women, who have almost twice the amount of visceral adipose tissue as premenopausal women (Figure 2).2,3 This accumulation of abdominal fat is strongly associated with metabolic alterations, including lipoprotein concentrations. The lipid profile seen in patients with visceral obesity is the main feature of the metabolic syndrome.2,3 In our study men had more visceral fat, lower plasma high-density lipoprotein (HDL) cholesterol, higher triglycerides and higher insulin and blood glucose than women.2 In visceral obesity, low-density lipoprotein (LDL) cholesterol levels are relatively normal but there are more LDL particles (as quantified by apolipoprotein B levels) that are smaller and denser than normal.3 On the basis of the evidence linking visceral adiposity to an atherogenic lipid profile, it is not surprising that abdominal obesity measured by the waist-to-hip ratio4,5 or by the more direct quantification of visceral fat accumulation by CT2 is associated with cardiovascular events.
Ratio between visceral fat and subcutaneous fat areas quantified by computed tomography in men and women in 161 individuals randomized from the community (77 men and 84 women).2
Visceral fat areas determined by computed tomography according to age in men (M) and women (W) in the 161 participants of the community study, 31.7% aged 40-49, 30.4% 50-59, 23.6% 60-69 and 14.3% ≥70 years.2
Statins reduce both cardiovascular events and mortality, but it is not established whether they are equally effective in both sexes, especially for primary prevention. One reason for this uncertainty is the under-representation of women in statin trials, and meta-analyses have lacked the statistical power to reliably compare the effectiveness of statins in women and men. There are gender differences in statin use and achievement of LDL cholesterol targets in primary and secondary prevention, although statin therapy is of similar effectiveness in men and women with similar risk of cardiovascular disease.6,7
Statins safely lower the incidence of major vascular events by about 20% for every 40 mg/dl reduction in LDL cholesterol, regardless of baseline cardiovascular risk.6 In the Cholesterol Treatment Trialists’ (CTT) Collaboration report on the effects of statin therapy on LDL cholesterol published in 2012,6 major vascular events and mortality were lowered similarly in both sexes. This patient-level meta-analysis, which included more than 170 000 participants (27% women) with a median follow-up of nearly five years, established the effectiveness of statins regardless of cardiovascular risk and suggested that statins were equally effective in both sexes in all risk strata.6 Subsequently, the same group analyzed the data in greater detail to describe the effects of statins in women and men separately.7 Statins had similar effects on lipid levels in women and men after one year of treatment. For each 40 mg/dl reduction in LDL cholesterol, women and men had comparable overall reductions in major vascular events and total mortality in both primary and secondary prevention settings.7
It is in this context that the results of the DISGEN-LIPID study are published in this issue of the Journal. In this observational cross-sectional study, the investigators noted that compared with men, women had significantly higher total and HDL cholesterol and lower triglyceride levels, although it should be noted that almost 94% of them were post-menopausal.8 In this descriptive study, more than half of the high or very high risk patients had not achieved the recommended lipid goals. In these risk strata, women were less well controlled than men (37% vs. 43%). The good news is that DISGEN-LIPID did not observe gender differences in dyslipidemia treatment in Portugal.8 This real-word study thus contributes to our overall understanding of atherogenic dyslipidemia.
Conflicts of interestThe author has no conflicts of interest to declare.