The clinical study of the range of diseases and other conditions affecting humans is complicated by a variety of factors that are at times inter-related. Thus, in order to establish causal relations, we need well-designed studies and powerful analytical tools. Randomized controlled clinical trials are considered to provide the best quality evidence, but they are not always appropriate, often for ethical reasons. Observational studies, if carefully designed, can provide results of similar quality to randomized trials,1,2 and prospective studies are less likely to suffer from bias and confounding factors.3 They are, however, more difficult to perform, may require longer follow-up periods to obtain sufficient observations, and are more costly to organize and run.3 Retrospective observational studies, on the other hand, take less time and are less expensive than prospective studies, but are more susceptible to bias in data selection and analysis.3
Of greater importance than study design is the quality of the data that support any study, since they are the foundation of its results and hence of its conclusions. When records are used that were not specifically designed for the study in question, the available data may be inadequate or of poor quality. In particular, there may be insufficient information on potential confounding factors. Poor quality data are a problem to which no institution is immune and sometimes cannot be effectively used.4 Although no dataset is perfect, retrospectively obtained data cause greater problems, mainly because the methods of acquiring variables were not established before the study commenced.
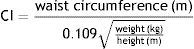
Various anthropometric indices have been used to assess the risk of developing disease, including body mass index, waist circumference and waist-to-hip ratio. In 1991, Rodolfo Valdez proposed the conicity index (CI) to assess obesity and body fat distribution, on the grounds that central rather than general obesity is associated with cardiovascular disease.5 CI is calculated using waist circumference and height in m and weight in kg by the following formula:
The article by Fontela et al. entitled “Study of conicity index, body mass index and waist circumference as predictors of coronary artery disease” in this issue of the Journal6 is a retrospective observational longitudinal study of individuals seen at the Cruz Alta Cardiology Institute (ICCA), Rio Grande do Sul, Brazil, between 2001 and 2012. The data were obtained from the “general patient registry” of the institute, which had been “maintained by a cardiologist since 2001”. This casts considerable doubt on the study's internal validity, since it is difficult to assess the possibility of selection and information bias, the quality of follow-up, and the presence of confounding factors. The authors attempted to overcome these limitations by setting inclusion and exclusion criteria, defining primary and secondary endpoints, analyzing confounding factors, validating collection of data from the “general patient registry” and performing a careful statistical analysis. Nevertheless, the shortcomings described above mean that the study's conclusions cannot be generalized.
Unlike Fontela et al., a study by Pitanga and Lessa,7 on the sensitivity and specificity of the conicity index in discriminating coronary risk, was a cross-sectional study of a probabilistic sample of adults in Salvador, Brazil that used a previously defined and tested methodology. Ten field investigators and two supervisors, both nutritionists, were trained in all aspects of the study, and performed an initial analysis to test the methodology and to refine the instruments and techniques, including the dynamics of the fieldwork. In this test, 100 participants in 50 residences were visited, and interviews and exams were carried out according to the established methodology. This test group was not included in the study sample.7
The VALSIM study, an epidemiological study of the prevalence of metabolic syndrome and its components in Portugal, was a cross-sectional analysis of a representative sample of adults resident in mainland Portugal and the islands of Madeira and the Azores attended in a primary health care setting.8 It concluded that the prevalence of metabolic syndrome in Portugal is high (27.5%) and is strongly linked to the occurrence of cardiovascular disease, and in particular to diabetes.8 A substudy of VALSIM found that the prevalence of obesity or overweight among diabetic patients was 84.6% and that the prevalence of abdominal obesity as defined by the National Cholesterol Education Program Adult Treatment Panel III criteria was 69.3%.9
Cardiovascular disease is the leading cause of mortality and morbidity worldwide, and its prevalence is expected to rise in the next decade, mainly due to demographic changes but also because of increasingly sedentary lifestyles and the rising prevalence of obesity and diabetes. Against this background, the conicity index, which has as yet been little studied, merits closer attention, and so the study by Fontela et al. is interesting but, as the authors point out, its “results should be considered exploratory and need to be confirmed in future studies”.
Conflicts of interestThe author has no conflicts of interest to declare.
Please cite this article as: Rato Q. Índice de conicidade: uma medida antropométrica a avaliar. Rev Port Cardiol. 2017;36:365–366.