Obesity is a major risk factor for cardiovascular disease. This study was designed to assess whether the conicity index (CI), body mass index (BMI) and waist circumference (WC) can be used as predictors of coronary artery disease (CAD) and mortality in a middle-aged population of the north-western region of Rio Grande do Sul, Brazil.
MethodsThis was a retrospective, longitudinal cohort study, based on the medical records of patients seen in a cardiology institution in a rural area of Rio Grande do Sul. The sample consisted of 2396 individuals. The primary endpoint was diagnosis of CAD, with mortality as the secondary endpoint. CI, BMI and WC were assessed using logistic regression, Cox regression and receiver operating characteristic curve analysis.
ResultsThe study showed that none of the anthropometric measures could be considered independent factors for either a diagnosis of CAD or mortality. Female gender was associated with a significantly lower risk of CAD (odds ratio [OR]: 0.31; 95% confidence interval [CI]: 0.22-0.44), as was absence of diabetes (OR: 0.52; 95% CI: 0.33-0.82), while there was a significantly higher risk of mortality associated with the presence of CAD (OR: 3.56; 95% CI: 2.00-6.32) and alcohol consumption (OR: 3.55; 95% CI: 1.60-7.90).
ConclusionsThese anthropometric measures were not independent predictive factors for CAD diagnosis or mortality in a population in southern Brazil. Our results support the conclusion that determination of CI, BMI and WC alone is insufficient to assess the risk of CAD and mortality in the general population.
A obesidade é um importante fator de risco para doenças cardiovasculares. O objetivo deste estudo foi avaliar se o índice de conicidade (IC), índice de massa corporal (IMC) e circunferência abdominal (CA) podem ser usados como preditores de doença arterial coronariana (DAC) e mortalidade em uma população de meia-idade da região noroeste do Rio Grande do Sul, Brasil.
MétodosEstudo de coorte retrospectiva, longitudinal, realizado com o registro dos prontuários de indivíduos atendidos em uma instituição cardiológica do interior do Rio Grande do Sul, Brasil. A amostra constou de 2396 indivíduos. Foram consideradas como variáveis de desfecho primário o diagnóstico de DAC e secundário a mortalidade. O IC, IMC e CA foram analisados através de regressão logística, regressão de Cox e curva ROC.
ResultadosO estudo mostrou que nenhuma das medidas antropométricas pôde ser considerada como fatores independentes, tanto para o diagnóstico de DAC, quanto para a mortalidade. Houve uma redução significativa do risco para DAC associada com o sexo feminino (odds ratio [OR]: 0,31; intervalo de confiança [IC95%]: 0,22-0,44) e ausência de diabetes mellitus (OR: 0,52; IC95%: 0,33-0,82) e um aumento significativo do risco de mortalidade associada à presença de DAC (OR: 3,56; IC95%: 2,00-6,32) e etilismo (OR: 3,55; IC95%: 1,60-7,90).
ConclusãoAs medidas antropométricas não se mostraram importantes como fator preditivo independente para o diagnóstico de DAC e mortalidade em uma população estudada no sul do Brasil. Nossos resultados suportam o conceito de que a mensuração isolada do IC, IMC e CA não são suficientes na avaliação do risco de DAC e mortalidade na população geral.
The incidence of many chronic diseases is high among obese individuals and the distribution of body fat has been the subject of research on obesity, since the metabolic and cardiovascular repercussions tend to be more severe when body fat is centralized, i.e. concentrated in the abdominal region.1,2
There is consensus that abdominal obesity is in turn related to the amount of visceral adipose tissue, and is an independent risk factor for cardiovascular disease.3–5 Visceral fat is metabolically more active than subcutaneous fat6 and correlates closely with insulin resistance.6–8 Excessive abdominal fat is associated with various metabolic disorders and with higher morbidity and mortality from atherosclerotic conditions such as coronary artery disease (CAD).9,10
The best anthropometric measure to assess the risk associated with obesity has not been established. Body mass index (BMI), obtained by dividing a person's weight in kg by the square of their height in m, is the measure of general obesity most commonly used in epidemiological studies,11 but it has been suggested that fat mass distribution is a better predictor of disease than general obesity.11,12
Waist circumference (WC), a measure of both subcutaneous and visceral fat, is easily determined and is frequently used as a measure of abdominal adiposity in epidemiological studies.13,14 WC is a more effective measure of body fat than BMI,11 since it correlates strongly with visceral fat, which is harmful to health.12
In 1991 Valdez15 proposed the conicity index (CI) as a model to assess obesity and body fat distribution. This includes the variables of weight, height and WC, thus weakening the correlation between WC and height, on the grounds that central rather than general obesity is associated with risk for cardiovascular disease. This model is based on the idea that the body shape of people who accumulate fat in the abdominal region resembles a double cone with a common base, while the shape of those with less fat in this central region resembles a cylinder.16
Pitanga and Lessa16 reported that CI had high sensitivity and specificity in assessing CAD risk in a cross-sectional study of adults in Salvador, Brazil. However, there are no studies demonstrating the same results in other Brazilian populations, or longitudinal studies confirming that CI can routinely be used as a predictor of CAD.
The present study was thus designed to determine whether the findings of Pitanga and Lessa could be reproduced,16 as well as to assess whether BMI and WC can be used as predictors of CAD and mortality in a middle-aged population of the north-western region of Rio Grande do Sul, Brazil.
MethodsThe study was approved by the ethics committee of Universidade de Cruz Alta (UNICRUZ) (0068.0.417.000-09) in accordance with the Declaration of Helsinki.
This was a retrospective longitudinal cohort study based on the medical records of patients seen in a cardiology institution in a rural area of Rio Grande do Sul, Brazil between 2001 and 2012. The study's endpoints were diagnosis of coronary events, presence of myocardial ischemia, and diagnosis of CAD, in a mean follow-up of 7.70±1.95 years.
Data collectionThe data were collected from the general patient registry of the Cruz Alta Cardiology Institute (ICCA), maintained by a cardiologist since 2001, on 6050 consecutive patients between 2001 and 2012. The population consisted of individuals seen at the Institute, which provides local and regional cardiological consultations for the prevention, diagnosis and treatment of cardiovascular disease. The ICCA has a research partnership with the Multidisciplinary Health Group at UNICRUZ and is registered with the Brazilian National Council for Scientific and Technological Development as a private institution engaged in clinical research.
All individuals were included who had complete data on the variables in the endpoints, namely anthropometric data for the calculation of CI, BMI and WC and records of myocardial ischemia or coronary events, as well as history of conventional cardiovascular risk factors and survival data. Individuals with other cardiomyopathies, valve disease or conduction system disorders were excluded, as were those aged <30 years since these have a low prevalence of atherosclerotic disease. This resulted in a sample of 2396 patients.
The primary endpoint was a diagnosis of CAD and/or the presence of myocardial ischemia. A diagnosis of CAD was based on a history of hospitalization for acute coronary syndrome, percutaneous or surgical myocardial revascularization documented by procedure reports, discharge notes or specialist reports. A diagnosis of myocardial ischemia was based on characteristic findings on functional tests and imaging exams.17,18 The secondary endpoint was all-cause mortality.
CI, BMI and WC were assessed as predictors, together with CAD risk factors including smoking, alcohol consumption, sedentary lifestyle, history or diagnosis of systemic hypertension, diabetes, hypercholesterolemia, hypertriglyceridemia, and family history of premature myocardial infarction.17
The data used to calculate CI, BMI and WC were recorded during anthropometric assessment at the ICCA. Body weight was measured in kg on a Toledo® scale, with the subject wearing light clothing and no shoes.19 Height was measured in m using a scale with 1-cm divisions, with the subject standing barefoot and facing forward. WC was measured at normal end-expiration at the midpoint between the last floating rib and the iliac crest, with the subject standing and wearing light clothing, using a flexible non-stretch tape measure with 1-mm divisions.19
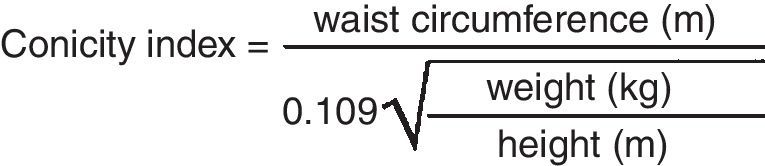
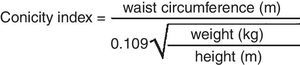
CI was calculated using the Valdez equation15 (Figure 1) based on the values for body weight, height and WC.
The conicity index proposed by Valdez15 to assess obesity and body fat distribution.
Epidemiological data were considered to be covariables, and included a history of diabetes, smoking, alcohol consumption, hypercholesterolemia, hypertriglyceridemia, systemic hypertension, sedentary lifestyle and metabolic syndrome.20 All individuals who said they smoked at the time of assessment were considered smokers, irrespective of the level of consumption, and those who reported excessive alcohol consumption around the time of the interview, irrespective of frequency, were considered to consume alcohol. A sedentary lifestyle was defined as less than 30 minutes’ exercise three times a week. The other variables were determined according to standard criteria.20–22
Statistical analysisTo check reliability, the records of 50 random individuals were examined by a different investigator and compared with the initially collected data. Inter-investigator agreement was tested using Cohen's kappa coefficient23 for categorical variables and the intraclass correlation coefficient for continuous variables.
Data were expressed as means ± standard deviation for continuous variables and as percentages for categorical variables. Individuals with and without CAD were compared using the Student's t test for parametric data and the Mann-Whitney test for non-parametric data for continuous variables, and the chi-square test for categorical variables. Multivariate linear logistic regression analysis was performed to determine changes in variables according to the presence or absence of a diagnosis of CAD. A Cox regression model which included duration of follow-up and adjusted for other variables was used to analyze mortality. Receiver operating characteristic (ROC) curve analysis was used to determine the specificity and sensitivity of CI and WC for the presence of CAD. A value of p<0.05 was considered significant.
ResultsOn analysis of data reliability, categorical variables presented kappa coefficients between 0.62 and 0.92 (p<0.001). Intraclass correlation coefficients for continuous variables ranged between 0.83 and 0.99 (p<0.001), confirming the reliability of the data obtained, since all variables were tested.
Descriptive statistics were used to characterize the sample, which consisted of 2396 individuals, 1440 female (60.1%) and 956 male (39.9%); 161 (6.7%) were diagnosed with CAD and 103 (4.3%) died, 2293 (95.7%) surviving to the end of follow-up. Most did not have diabetes (n=2127; 88.8%), hypercholesterolemia (n=1542; 64.4%) or hypertriglyceridemia (n=1751; 73.1%) or smoke (n=2040; 85.1%). Hypertension was observed in 1091 (45.5%) and most had a sedentary lifestyle (n=1745; 72.8%).
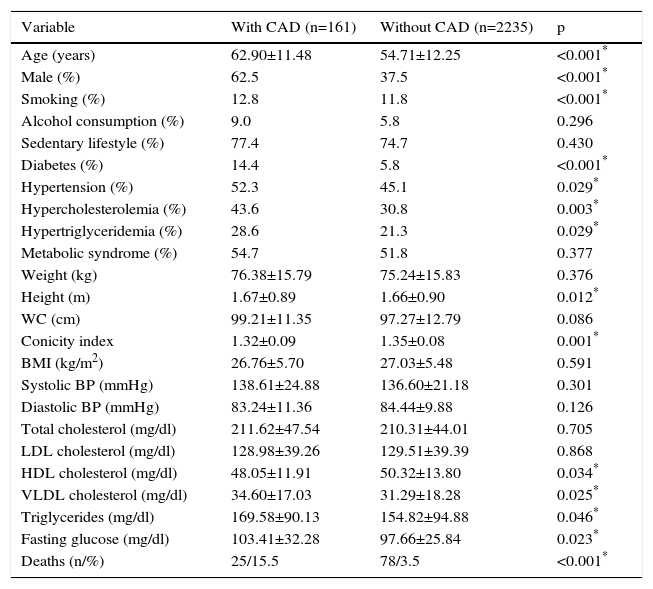
Analysis of the study population according to the presence of CAD (Table 1) showed that those with CAD were on average older, more often male, and with higher prevalences of diabetes, hypercholesterolemia, hypertriglyceridemia and hypertension. CI was significantly lower in the group with CAD. Levels of very low density lipoprotein cholesterol, triglycerides and blood glucose were higher, and high density lipoprotein cholesterol levels were lower, in those with CAD. The CAD group had higher mortality during follow-up.
Characterization of the study population (n=2396) according to the presence of coronary artery disease.
| Variable | With CAD (n=161) | Without CAD (n=2235) | p |
|---|---|---|---|
| Age (years) | 62.90±11.48 | 54.71±12.25 | <0.001* |
| Male (%) | 62.5 | 37.5 | <0.001* |
| Smoking (%) | 12.8 | 11.8 | <0.001* |
| Alcohol consumption (%) | 9.0 | 5.8 | 0.296 |
| Sedentary lifestyle (%) | 77.4 | 74.7 | 0.430 |
| Diabetes (%) | 14.4 | 5.8 | <0.001* |
| Hypertension (%) | 52.3 | 45.1 | 0.029* |
| Hypercholesterolemia (%) | 43.6 | 30.8 | 0.003* |
| Hypertriglyceridemia (%) | 28.6 | 21.3 | 0.029* |
| Metabolic syndrome (%) | 54.7 | 51.8 | 0.377 |
| Weight (kg) | 76.38±15.79 | 75.24±15.83 | 0.376 |
| Height (m) | 1.67±0.89 | 1.66±0.90 | 0.012* |
| WC (cm) | 99.21±11.35 | 97.27±12.79 | 0.086 |
| Conicity index | 1.32±0.09 | 1.35±0.08 | 0.001* |
| BMI (kg/m2) | 26.76±5.70 | 27.03±5.48 | 0.591 |
| Systolic BP (mmHg) | 138.61±24.88 | 136.60±21.18 | 0.301 |
| Diastolic BP (mmHg) | 83.24±11.36 | 84.44±9.88 | 0.126 |
| Total cholesterol (mg/dl) | 211.62±47.54 | 210.31±44.01 | 0.705 |
| LDL cholesterol (mg/dl) | 128.98±39.26 | 129.51±39.39 | 0.868 |
| HDL cholesterol (mg/dl) | 48.05±11.91 | 50.32±13.80 | 0.034* |
| VLDL cholesterol (mg/dl) | 34.60±17.03 | 31.29±18.28 | 0.025* |
| Triglycerides (mg/dl) | 169.58±90.13 | 154.82±94.88 | 0.046* |
| Fasting glucose (mg/dl) | 103.41±32.28 | 97.66±25.84 | 0.023* |
| Deaths (n/%) | 25/15.5 | 78/3.5 | <0.001* |
BMI: body mass index; BP: blood pressure; CAD: coronary artery disease; HDL: high density lipoprotein; LDL: low density lipoprotein; VLDL: very low density lipoprotein; WC: waist circumference. Data expressed as means ± standard deviation or percentages; Student's t test and Mann-Whitney test for continuous and chi-square test for categorical variables.
* Statistically significant.
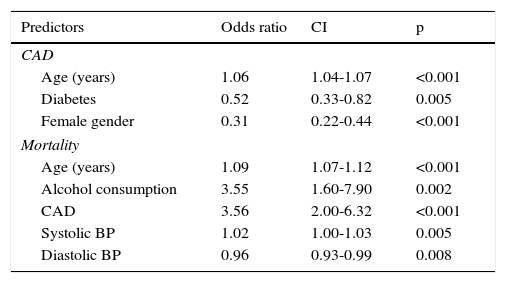
Table 2 shows the logistic regression models used to determine the variables that were predictors of a diagnosis of CAD and mortality. For the former, conventional risk factors such male gender, history of diabetes and advanced age remained significant in the final regression model and were shown to be associated with CAD in this sample. The data show that female gender and absence of diabetes are significant predictors for the absence of CAD. The likelihood of women in this population being diagnosed with CAD was 69.0% lower than in men, and the likelihood of CAD in those without diabetes was 48.0% lower than in those with diabetes.
Results of multivariate logistic regression for coronary artery disease and Cox regression for mortality.
| Predictors | Odds ratio | CI | p |
|---|---|---|---|
| CAD | |||
| Age (years) | 1.06 | 1.04-1.07 | <0.001 |
| Diabetes | 0.52 | 0.33-0.82 | 0.005 |
| Female gender | 0.31 | 0.22-0.44 | <0.001 |
| Mortality | |||
| Age (years) | 1.09 | 1.07-1.12 | <0.001 |
| Alcohol consumption | 3.55 | 1.60-7.90 | 0.002 |
| CAD | 3.56 | 2.00-6.32 | <0.001 |
| Systolic BP | 1.02 | 1.00-1.03 | 0.005 |
| Diastolic BP | 0.96 | 0.93-0.99 | 0.008 |
Waist circumference, body mass index, conicity index, hypercholesterolemia, hypertriglyceridemia, hypertension, sedentary lifestyle, metabolic syndrome, total, LDL, HDL and VLDL cholesterol, and smoking did not remain in the model due to p>0.05.
BP: blood pressure; CAD: coronary artery disease; CI: confidence interval.
Analysis of predictors of mortality, after adjustments in the Cox regression model to take account of duration of follow-up, showed that the presence of CAD increased the likelihood of death by 3.56 times, as did alcohol consumption. Age and blood pressure levels had less of an effect.
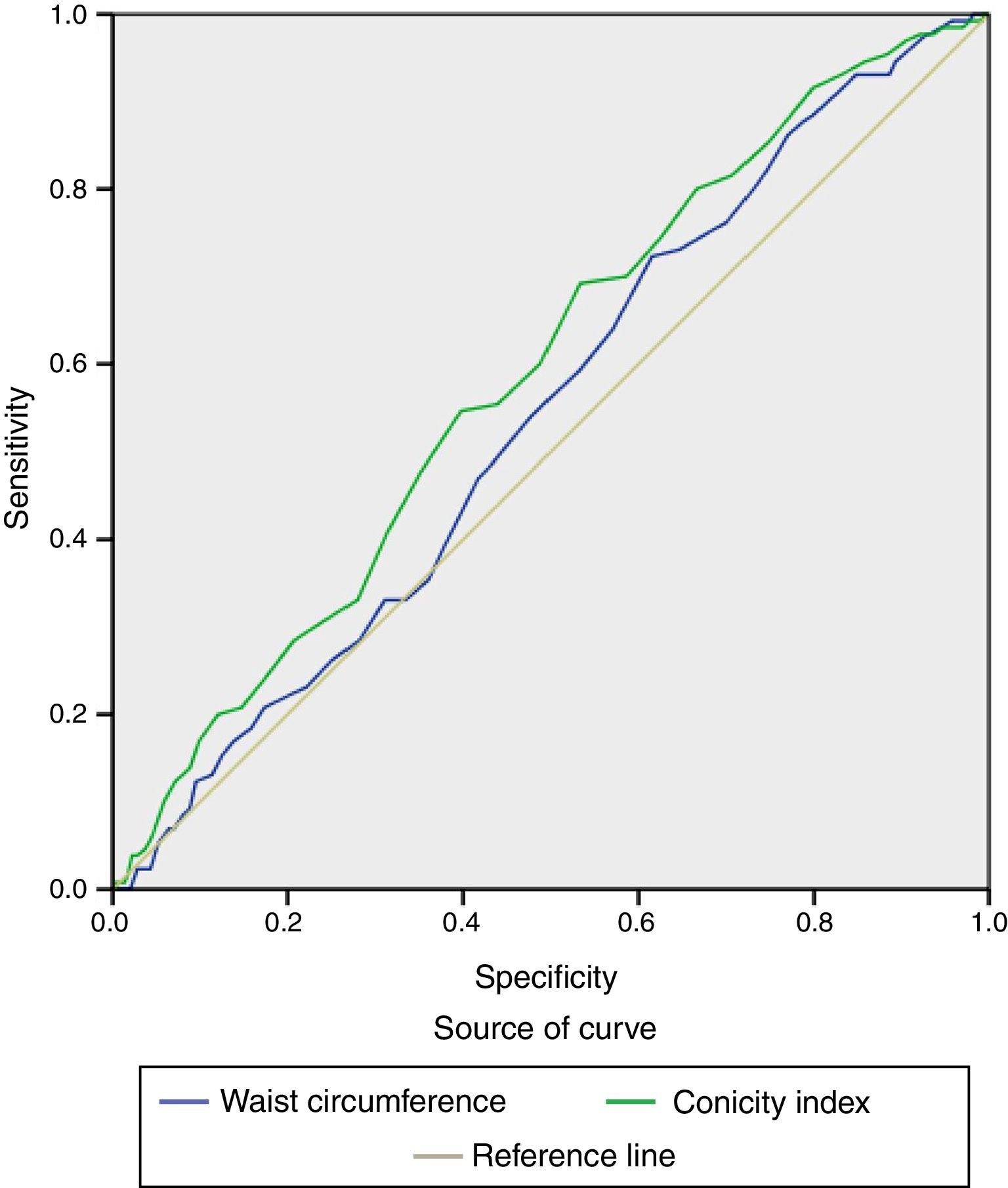
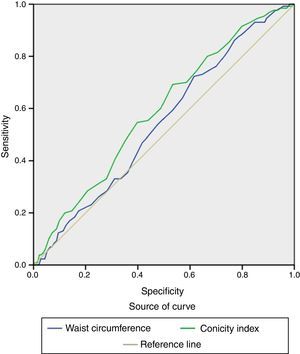
CI, BMI and WC were not included in the regression model and could not therefore be considered independent predictors of CAD or mortality in the study population. Furthermore, supporting these findings, the results of ROC analysis revealed low specificity and sensitivity, as shown in Figure 2. The areas under the ROC curve for WC and CI were 0.57 (0.49-0.59; p=0.007) and 0.59 (0.54-0.63; p=0.001), respectively.
DiscussionThe present study is the first longitudinal study of a population from the south of Brazil to show that BMI, WC and CI are not predictors of CAD or mortality in a sample including both sexes, with and without CAD. Anthropometric measures are widely recommended to stratify cardiovascular disease risk, probably due to their ease of measurement. However, in this study population, based on different regression models for two endpoints, these anthropometric measures were not associated in the final logistic regression model with either CAD or mortality. Our results support the idea that determination of IC, BMI and WC alone is insufficient to assess the risk of CAD and mortality in the general population.
Conflicting findings concerning associations between measures of central obesity and CAD and mortality were the rationale for the present study. Pitanga and Lessa,16 assessing the sensitivity and specificity of CI as a predictor of coronary risk in Brazilian adults, calculated areas under the ROC curve of 0.80 and 0.75 for men and women, respectively, and suggested that this index should be compared with other anthropometric indicators of obesity. The present study compared CI with BMI and WC, but found that none of the measures was associated with a diagnosis of CAD or mortality in a cohort of the general population. Furthermore, the area under the ROC curve for CI was less than that reported by Pitanga and Lessa.16
In specific populations, such as women, longitudinal studies14,24 conducted in subgroups of the 1976 Nurses’ Health Study cohort consisting of nurses aged 30-55 years, with no history of CAD, stroke or cancer, resident in eleven US states, demonstrated that measures of abdominal adiposity were predictive of CAD irrespective of BMI. Some cross-sectional studies25,26 have suggested that waist-to-height ratio may be superior to BMI and waist-to-hip ratio in predicting cardiovascular risk. These studies demonstrated that waist-to-height ratio was better at predicting hypertension and diabetes than BMI and waist-to-hip ratio in a sample of 4923 individuals aged ≥20 years living in a rural area,25 and was a better predictor of multiple CAD risk factors than waist-to-hip ratio in a sample of 3131 men.26
A case-control study of myocardial infarction in India27 with 100 participants (50 cases and 50 controls) showed a significantly increased risk for CAD associated with visceral fat area (OR: 5.67; 95% CI: 1.96-16.95), waist-to-hip ratio (OR: 7.07; 95% CI: 2.19-24.27), WC (OR: 2.63; 95% CI: 1.05-6.66) and BMI (OR: 2.53; 95% CI: 1.03-6.26). However, the small sample size and extremely wide confidence intervals were a major limiting factor of this series; in addition, the study was conducted in a foreign population.
The American Heart Association's scientific statement on assessing adiposity28 stressed that while BMI generally correlates well with body fat in the population as a whole, there are significant individual differences that are related to various factors, including age, gender, genetics and ethnicity and race, but also arise from differences in body fat distribution and composition. Thus, while BMI is a good initial measure, it is certainly not sufficient in clinical terms, and so it is important to consider the use of other simple clinical tools than can help identify high-risk individuals with excess visceral fat by providing additional information on adiposity and risk of associated comorbidities.28 It therefore appears there is no single anthropometric measure that is able to predict a diagnosis of CAD, which may explain why we found no association between CI, BMI or WC with CAD in the general population.
Central obesity has been shown to predict mortality in longitudinal studies in the general population29,30 and in patients with CAD.31,32 In the case of the general population, BMI values in the overweight and obese bands are associated with higher overall mortality, as demonstrated in collaborative analyses33 of 57 prospective studies in 894576 individuals with no history of heart disease, mainly in Western Europe and North America. However, in a systematic review and meta-analysis34 of 40 cohort studies with a total of 250152 individuals with CAD, the highest BMI band (30-35) was associated with lower total mortality (OR: 0.93; 95% CI: 0.85-1.03) and cardiovascular mortality (OR: 0.97; 95% CI: 0.82-1.15). This has been termed the obesity paradox; these findings may be explained by the inability of BMI to differentiate between body fat and lean mass, since the analyses were adjusted for confounding factors.
A recent study35 of 15547 individuals with CAD using Cox proportional hazard models that adjusted for potential confounders to assess mortality risk according to different patterns of adiposity and that combined BMI with measures of central obesity showed that individuals with CAD with normal BMI but central obesity as assessed by WC and waist-to-hip ratio have worse survival compared with subjects with other adiposity patterns. In a retrospective study of 285 patients with myocardial infarction or unstable angina in Portugal,36 introducing WC into the GRACE risk score did not add prognostic information on mortality or reinfarction at six-month follow-up, and thus abdominal obesity was not shown to have prognostic value in acute coronary syndrome. The population in the Portuguese study presented a rate of abdominal obesity of 44.6%, lower than found in the present study (57.2%), defined in both studies according to the National Cholesterol Education Program Adult Treatment Panel III cut-offs of >88 cm for women and >102 cm for men.21 In the present study, the measures were applied separately rather than in combinations, which may explain why no measure was associated with mortality as each measure has its limitations, and combining such measures is not appropriate due to the multicollinearity between BMI, WC and CI, which are based on the same variables and therefore cannot be used in combination to predict risk of CAD or mortality.
The main limitation of the present study is its retrospective and single-center nature, although the robustness of the database, together with the length of follow-up and longitudinal design, would tend to reduce this limitation. Moreover, male gender, diabetes and advanced age were shown to be risk factors for CAD, an association that has been thoroughly corroborated by longitudinal studies on the Framingham Heart Study cohort,37–40 as has the association between CAD and alcohol consumption and mortality.
Our results may help to refine practice in terms of obesity in the general population, since they highlight the fact that anthropometric measures alone are insufficient to predict a diagnosis of CAD or mortality. Identifying individuals with greater abdominal adiposity does not appear to be of major importance in efforts to prevent cardiovascular disease, although it is still necessary for monitoring and controlling other conditions such as metabolic syndrome and its components. None of the measures assessed was able to predict CAD or mortality in this study population. Nevertheless, our results should be considered exploratory and need to be confirmed in future studies.
ConclusionThe anthropometric measures assessed in this study were not independent predictive factors for a diagnosis of CAD or mortality in a population in southern Brazil. Our results support the conclusion that determination of IC, BMI and WC alone is insufficient to assess the risk of CAD and mortality in the general population.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Caitano Fontela P, Winkelmann ER, Nazario Viecili PR. Estudo do índice de conicidade, índice de massa corporal e circunferência abdominal como preditores de doença arterial coronariana. Rev Port Cardiol. 2017;36:357–364.