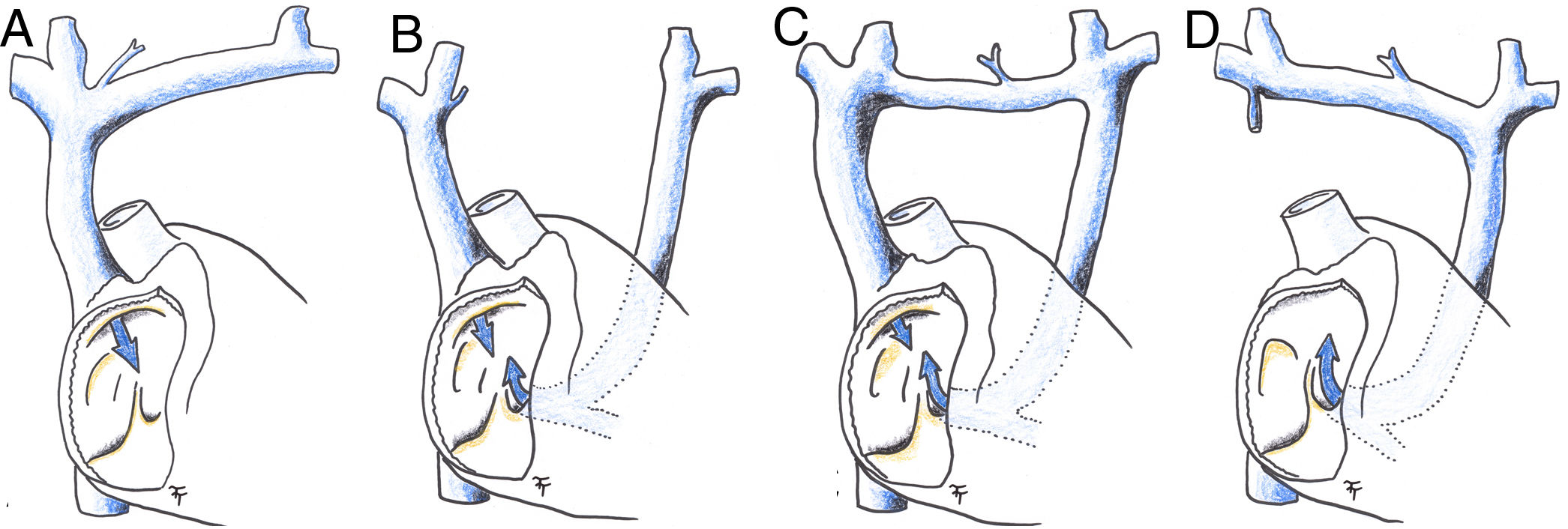
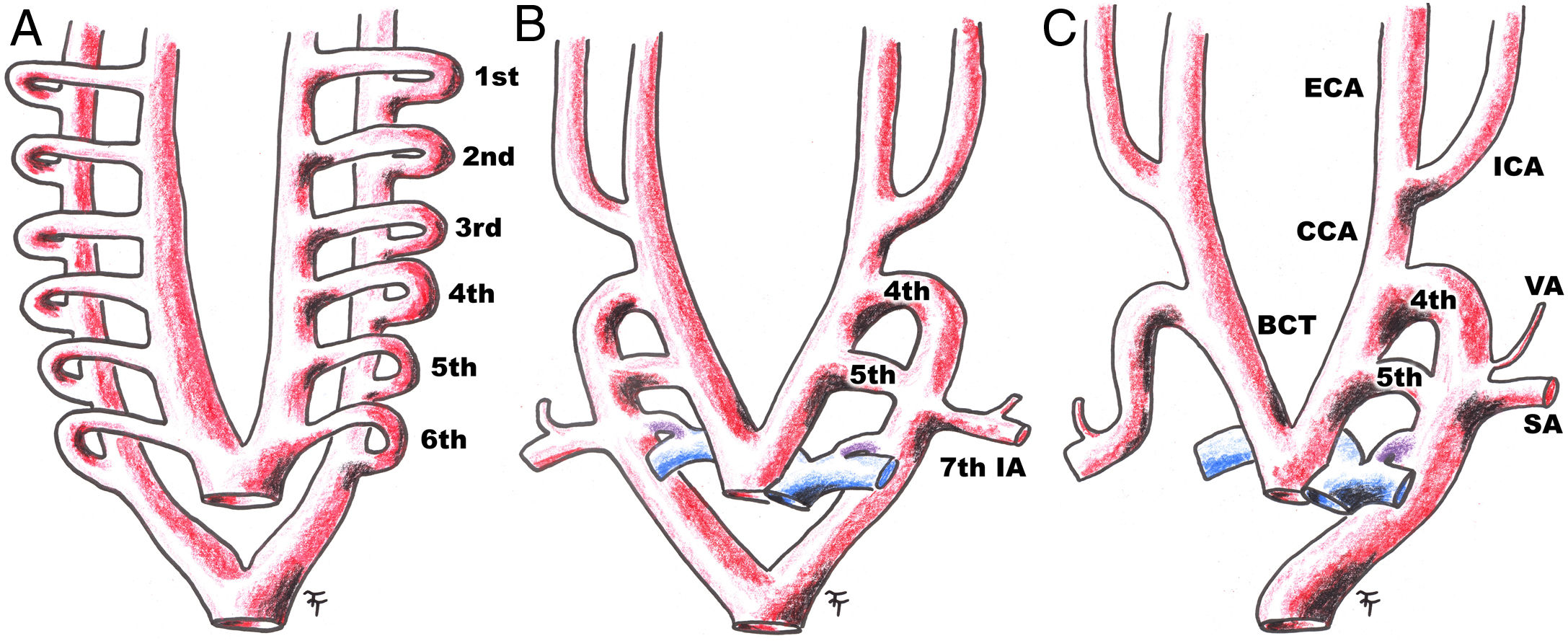
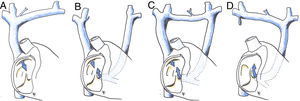
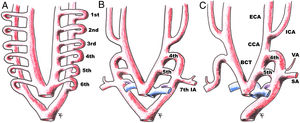
Persistent left superior vena cava (LSVC) is the most common venous anomaly, with an incidence of 0.3-0.5% in the general population.1 However, absence of the right superior vena cava (RSVC) is found in only 10-20% of cases (Figure 1).1,2 A double-lumen aortic arch is one of the rare aortic anomalies caused by the persistence of the fifth aortic arch (Figure 2).3 A unicuspid aortic valve (UAV) was first described by Edwards in 1958, and the incidence of this rare malformation in the population is 0.02%.4,5
Diagram of superior vena cava anomalies. (A) Physiological right superior vena cava; (B) persistent left superior vena cava; (C) persistent left superior vena cava with an anterior communicating vein; (D) persistent left superior vena cava and absent right superior vena cava. Blue arrow: intake of deoxygenated blood from upper part of the body into the right atrium.
Diagram of the embryonic development of a double-lumen aorta with a persistent fifth aortic arch, with progression from A to C. 1st: first aortic arch; 2nd: second aortic arch; 3rd: third aortic arch; 4th: fourth aortic arch; 5th: fifth aortic arch; 6th: sixth aortic arch; 7th IA: seventh intersegmental artery; BCT: brachiocephalic trunk; CCA: common carotid artery; ECA: external carotid artery; ICA: internal carotid artery; SA: subclavian artery; VA: vertebral artery.
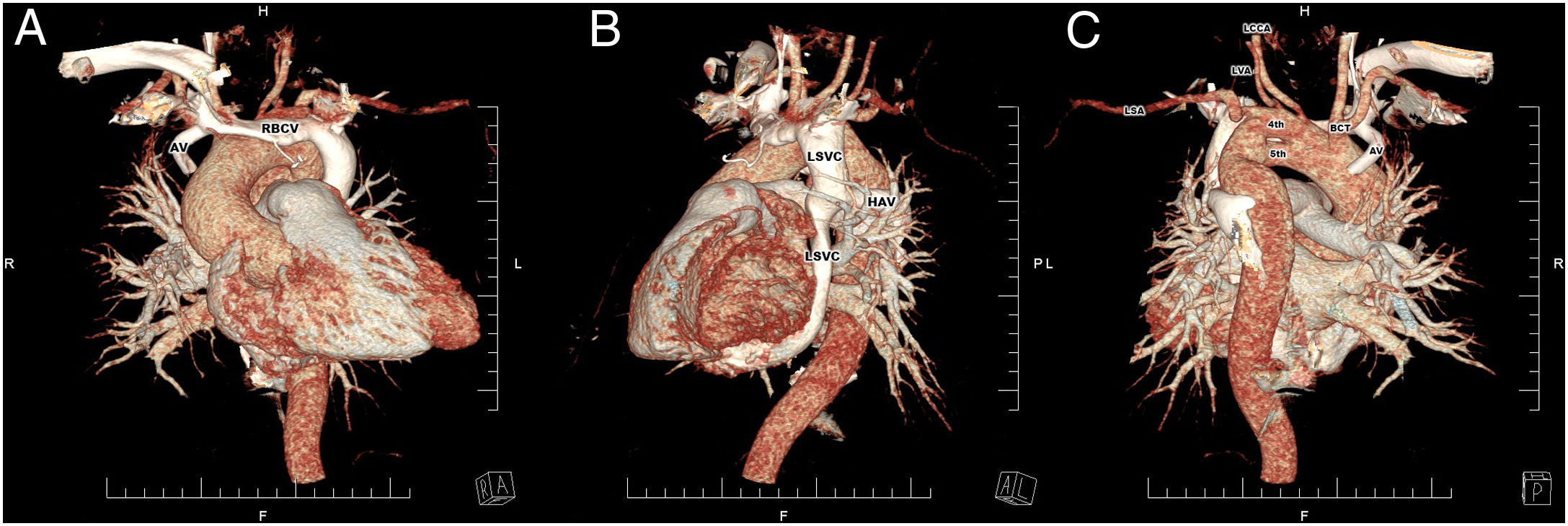
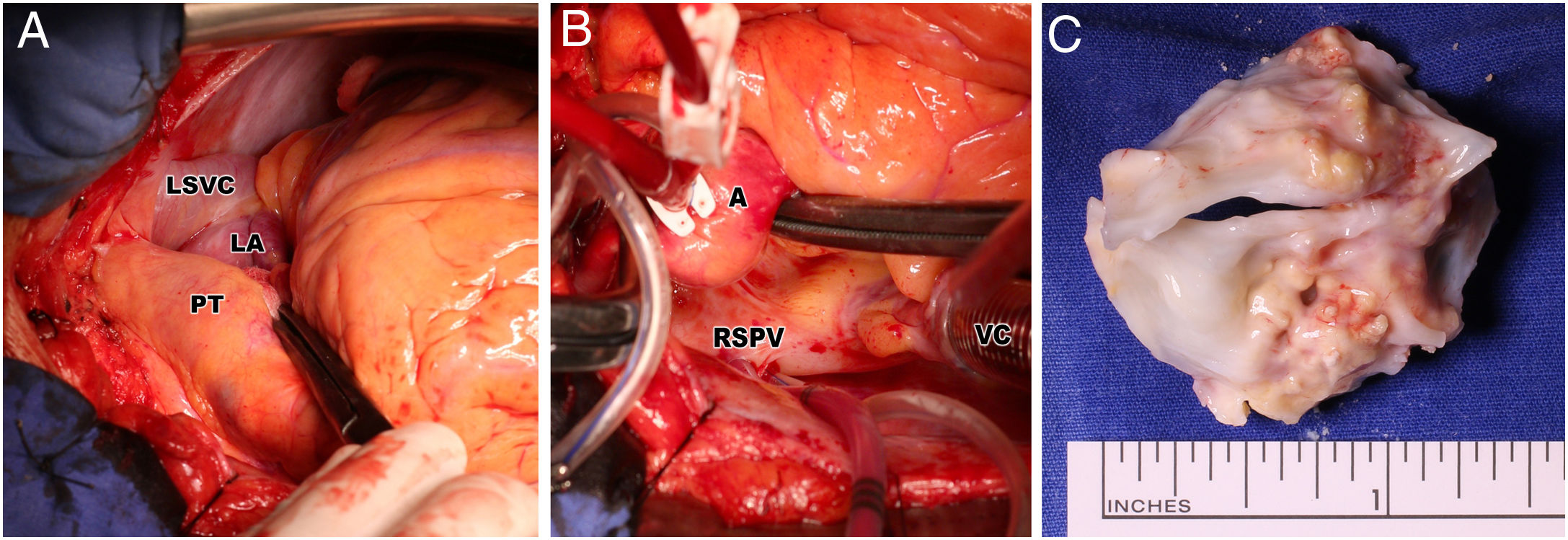
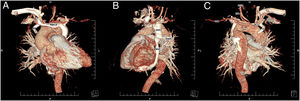
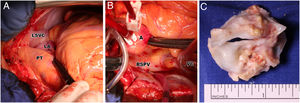
We report the case of a 36-year-old man with a persistent LSVC, an absent RSVC, a double-lumen aortic arch, probably caused by a persistent fifth aortic arch, and a stenotic UAV (peak gradient 92 mmHg, median gradient 46 mmHg and aortic valve area 0.92 cm2) (Figure 3). He reported stable angina pectoris and dyspnea during minimal exertion. Coronary angiography showed normal coronary arteries. Genetic study showed no deletion in 22q11.2. The patient underwent aortic valve replacement with implantation of a mechanical prosthesis (22-mm ATS) (Figure 4). Cardiopulmonary bypass was established under standard conditions with antegrade cardioplegia.
Three-dimensional computed tomography reconstruction of persistent left superior vena cava (A and B) and persistent fifth aortic arch (C). 4th: fourth aortic arch; 5th: fifth aortic arch; AV: azygos vein; BCT: brachiocephalic trunk; HAV: hemizygos vein; LCCA: left common carotid artery; LSA: left subclavian artery; LSVC: left superior vena cava; LVA: left vertebral artery; RBCV: right brachiocephalic vein.
Perioperative photograph of persistent left superior vena cava (A), absent right superior vena cava (B) and excised unicommissural unicuspid stenotic aortic valve (C). A: aorta; LA: left atrium; LSVC: left superior vena cava; PT: pulmonary trunk; RSPV: right superior pulmonary vein with the inserted venous cannula; VC: venous cannula of cardiopulmonary bypass inserted through the right atrium into the right atrium.
Despite the extent of the patient's congenital anomalies, the condition was completely asymptomatic in infancy and early adulthood. No surgery was necessary before the degeneration and progressive stenosis of the UAV. The authors expect the patient to remain free of symptoms, depending on continuing good function of the mechanical prosthesis.
Ethics approval and consent to participateThe Independent Ethics Committee of the Eastern Slovak Institute for Cardiovascular Diseases, Ltd. confirmed that the case report is in compliance with the principles of the Declaration of Helsinki and the ICH Guidelines for Good Clinical Practice and applicable regulatory requirements.
FundingThis article was supported in part by the Grant Agency of the Ministry of Education, Science, Research and Sport of the Slovak Republic (VEGA 1/0873/18).
Conflicts of interestThe authors have no conflicts of interest to declare.
Consent for publicationInformed consent for publication of images from the surgery was obtained, and the records on consent are available for the editor.