Wolff-Parkinson-White (WPW) syndrome is the most common manifestation of ventricular pre-excitation syndrome and is mostly found in individuals with no structural heart disease. Although the risk of malignant arrhythmias is low, sudden cardiac death (SCD) as the first clinical manifestation of WPW syndrome is well documented, and atrial fibrillation (AF) with a rapid ventricular response is the main mechanism involved. Unfortunately, the signs of pre-excitation and arrhythmias are sometimes under-diagnosed and under-treated. We describe the case of a 31-year-old man who was admitted with an irregular wide complex tachycardia consistent with pre-excited AF, which was not promptly diagnosed, and who developed ventricular fibrillation (VF) after administration of atrioventricular (AV) nodal blockers, as a primary manifestation of WPW syndrome. Blocking the AV node in patients with pre-excited AF may increase the ventricular rate and potentially result in hemodynamic instability. Among patients with WPW syndrome who survive an episode of SCD, catheter ablation of the accessory pathway is the treatment of choice.
A síndrome de Wolff-Parkinson-White (WPW) é a manifestação mais comum da síndrome de pré-excitação ventricular e está presente maioritariamente em indivíduos sem cardiopatia estrutural. Embora o risco de arritmias malignas seja baixo, a morte súbita cardíaca (MSC) como primeira manifestação clínica da síndrome de WPW é uma ocorrência bem documentada e a fibrilhação auricular (FA) com resposta ventricular rápida é o principal mecanismo envolvido. Infelizmente, às vezes, os sinais de pré-excitação e as arritmias são subdiagnosticados e subtratados. Descrevemos o caso de um homem de 31 anos admitido com uma taquicardia irregular de complexos largos consistente com FA pré-excitada, não diagnosticada de imediato, que evoluiu para fibrilhação ventricular (FV) após a administração de bloqueadores do nó auriculoventricular (AV), como manifestação inaugural da síndrome de WPW. O bloqueio do nó AV, em pacientes com FA pré-excitada, pode aumentar a frequência ventricular e potencialmente resultar em instabilidade hemodinâmica. Entre os pacientes com síndrome de WPW que sobrevivem a um episódio de MSC, a ablação por cateter de via acessória (VA) é o tratamento de escolha.
Wolff-Parkinson-White (WPW) syndrome refers to the association of manifest pre-excitation and symptoms due to reentrant arrhythmias. The risk of malignant arrhythmias is low but sudden cardiac death (SCD) may be the first manifestation of this condition.1 More frequently, these patients suffer from atrioventricular reentrant tachycardia (AVRT) and/or pre-excited atrial fibrillation (AF) with rapid anterograde conduction through an accessory pathway (AP) that can deteriorate into ventricular fibrillation (VF).2 Electrophysiological study (EPS) and radiofrequency ablation (RFA) of the AP is therefore recommended in symptomatic patients as it is a very effective treatment and can prevent a potentially fatal outcome.3
Case reportA 31-year-old man with no known cardiac disease, a family history of SCD in a paternal aunt and uncle in the 1950s, and a history of long-standing paroxysmal palpitations that resolved with vagal maneuvers (never documented on an electrocardiogram [ECG]), was admitted to the emergency department (ED) complaining of palpitations that persisted despite the usual Valsalva maneuvers. No medication or drug abuse was reported.
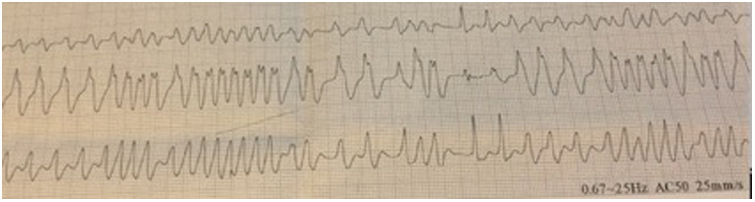
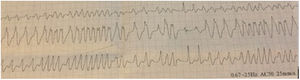
The patient was hemodynamically stable, with normal blood pressure (150/70 mmHg) and an irregular pulse approaching 200 bpm. The rest of the physical assessment was unremarkable, with no cardiac murmurs or signs of pulmonary edema. An ECG revealed an irregular wide complex tachycardia (Figure 1).
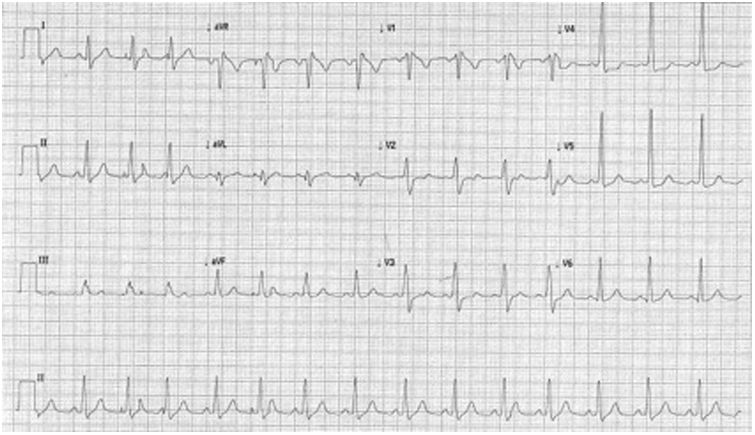
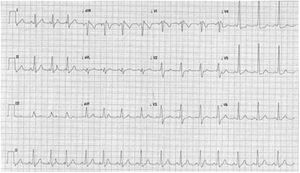
At the ED a decision was made to give intravenous adenosine (6+12+12 mg), followed by intravenous verapamil (2.5 mg). After the administration of these drugs, the patient developed VF which was reverted after two external defibrillator shocks (2×200 J, biphasic). A subsequent ECG showed a subtle pre-excitation pattern in the lateral leads, especially in V4-V5 (Figure 2). Laboratory parameters were normal and transthoracic echocardiography excluded structural heart disease.
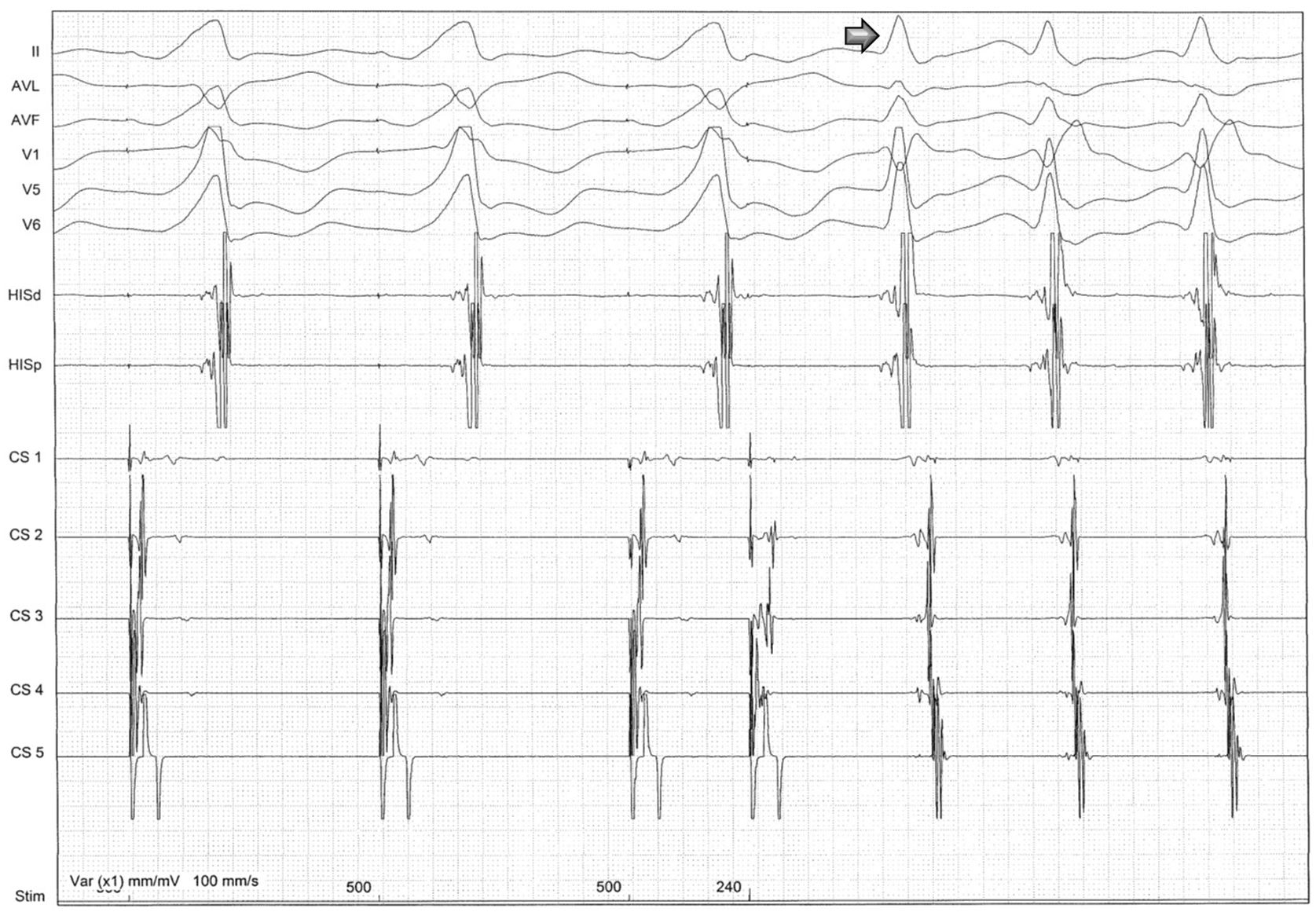
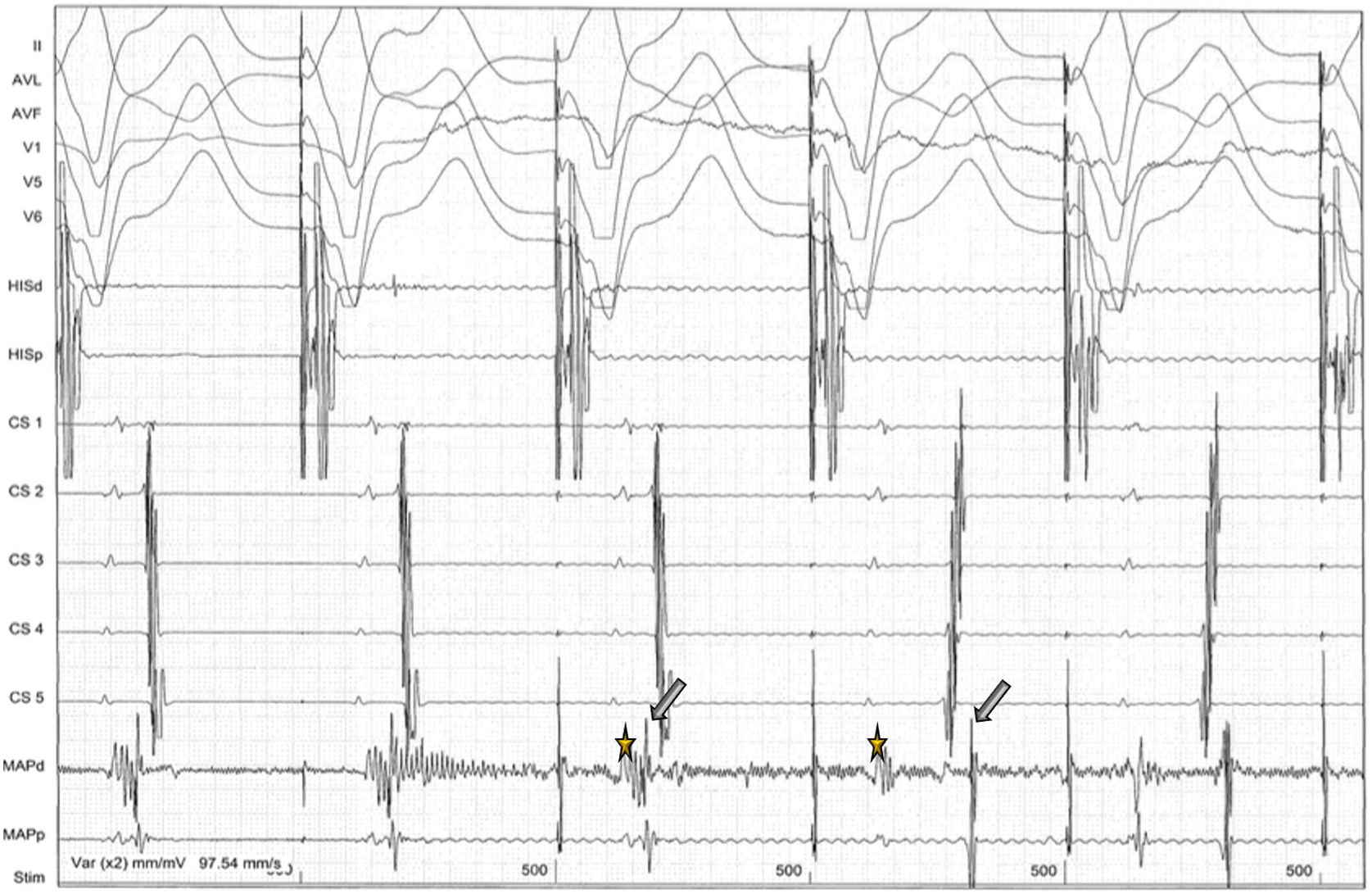
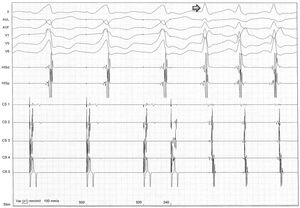
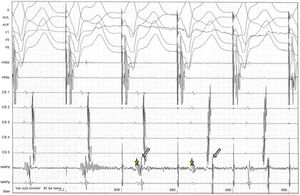
The patient was then referred for an EPS and a left lateral AP was diagnosed, capable of anterograde and retrograde conduction. Orthodromic AVRT was easily induced with both ventricular and atrial stimulation (Figures 3 and 4). The anterograde refractory period of the AP was 240 ms. Ablation of this pathway (Figure 5) was then successfully performed under ventricular pacing, the retrograde conduction through the AP disappearing immediately after starting radiofrequency (<3 s). Anterograde conduction was also confirmed to be absent after stopping radiofrequency. The procedure was uneventful and the subsequent ECG showed normal sinus rhythm (Figure 6).
After programmed ventricular pacing, the extra-stimulus maintained eccentric and non-decremental ventriculoatrial conduction up to 220 ms, and it was at this time, when the atrioventricular node was outside the refractory period and available for anterograde conduction, that orthodromic atrioventricular reentrant tachycardia was induced (arrow).
During programmed atrial pacing, atrioventricular conduction was performed through the accessory pathway until its anterograde refractory period (<240 ms) was reached. The impulse then proceeded to the ventricle via the atrioventricular node, leaving the accessory pathway available for retrograde conduction, and atrioventricular reentrant tachycardia had started (arrow).
The patient was discharged home on the following day. One month after RFA he was asymptomatic with a normal ECG tracing and no tachyarrhythmias were documented during this period.
DiscussionUnder physiological conditions, conduction from the atria to the ventricles occurs via the AV node and the His-Purkinje system. Patients with a pre-excitation syndrome have at least one AP that directly connects the atria and ventricles, thereby allowing electrical activity to bypass the AV node. Tissue in the AP typically conducts electrical impulses more quickly than the AV node, resulting in earlier activation of the ventricles, and is responsible for the classic ECG findings of a shortened PR interval (<0.12 s), slurring and slow rise of the initial QRS complex, and widened QRS complex (>0.12 s).
The prevalence of a WPW pattern on the surface ECG is estimated at 0.13–0.25% in the general population, but the prevalence of WPW syndrome is substantially lower.4 Diagnosis of WPW syndrome requires typical ECG findings with a documented dysrhythmia.
The most frequently found dysrhythmias in patients with WPW are AVRT and AF. Fortunately, the incidence of SCD in patients with WPW syndrome is quite low, ranging from 0.1 to 0.39%.3 Predicting clinical outcome is one of the major issues in WPW patients and remains a considerable clinical challenge. Risk factors for potentially life-threatening arrhythmic events in WPW syndrome5,6 include a short AP refractory period (<250 ms) allowing a rapid ventricular response in AF, inducibility of tachyarrhythmia during EPS (AVRT and/or AF), short pre-excited RR interval during AF (<250 ms), multiple APs, male gender, age and syncope.
In patients with an AP capable of anterograde conduction who develop AF, conduction to the ventricle often occurs through a combination of the normal conduction pathway (via the AV node) and the AP. However, because most APs have a shorter refractory period than the AV node, the ventricular rate can be more rapid if AV conduction occurs preferentially via the AP. Hence, AV nodal blocking drugs (adenosine, verapamil, beta-blockers, and digoxin) should be avoided in patients with pre-excited AF, since blocking the AV node will promote conduction down the AP, lengthening AV node refractoriness, and may sometimes directly increase the rate of conduction over the AP. Myocardial contractility and systemic vascular resistance will also be reduced, leading to a reflex increase in already elevated sympathetic tone that further shortens AP refractoriness.7–9
The goals of acute drug therapy for pre-excited AF are prompt control of the ventricular response and, ideally, reversion to sinus rhythm. If the patient is unstable because of a rapid ventricular response, electrical cardioversion should be performed. For more stable patients, trials of intravenous medications can be performed cautiously. Treatment of pre-excited AF requires a parenteral drug with rapid onset of action that lengthens anterograde refractoriness and slows conduction in both the AV node/His-Purkinje system and the AP, such as ibutilide or procainamide.3
Our case illustrates an example of an iatrogenic malignant arrhythmia in a WPW patient presenting with a pre-excited AF that was neither promptly diagnosed nor properly treated.
ConclusionPre-excited AF is a differential diagnosis that ED doctors should bear in mind when treating patients with irregular wide complex tachycardias. In these patients, AV nodal blocking drugs will promote conduction down the AP, increasing the risk of developing VF, and should therefore be avoided. Acute treatment of pre-excited AF should aim for control of ventricular rate and, ideally, reversion to sinus rhythm. The preferred long-term treatment approach is catheter ablation.
Conflicts of interestThe authors have no conflicts of interest to declare.