A 62-year-old woman was admitted with chest pain of two hours’ duration, ECG changes in the precordial leads and left ventricular ejection fraction of 30% on the echocardiogram. Emergent catheterization demonstrated severe flow disturbance in the left coronary artery. An intra-aortic balloon pump and a drug-eluting stent were implanted. However, the flow disturbance persisted. Optical coherence tomography followed by intravascular ultrasound provided crucial data on the mechanism and helped to optimize treatment in this critical patient.
Uma mulher de 62 anos foi internada devido a dor torácica com duas horas de duração, associada a alterações eletrocardiográficas nas derivações precordiais e FEVE: 30% determinada por ecocardiografia. Um cateterismo emergente revelou alterações graves no fluxo da coronária esquerda. Foram implantados um balão intra-aórtico e um stent revestido. Contudo, o fluxo continuou com alterações. A tomografia de coerência ótica e a ultrassonografia intravascular proporcionaram os dados únicos acerca do mecanismo envolvido e contribuíram para otimizar o tratamento numa doente crítica.
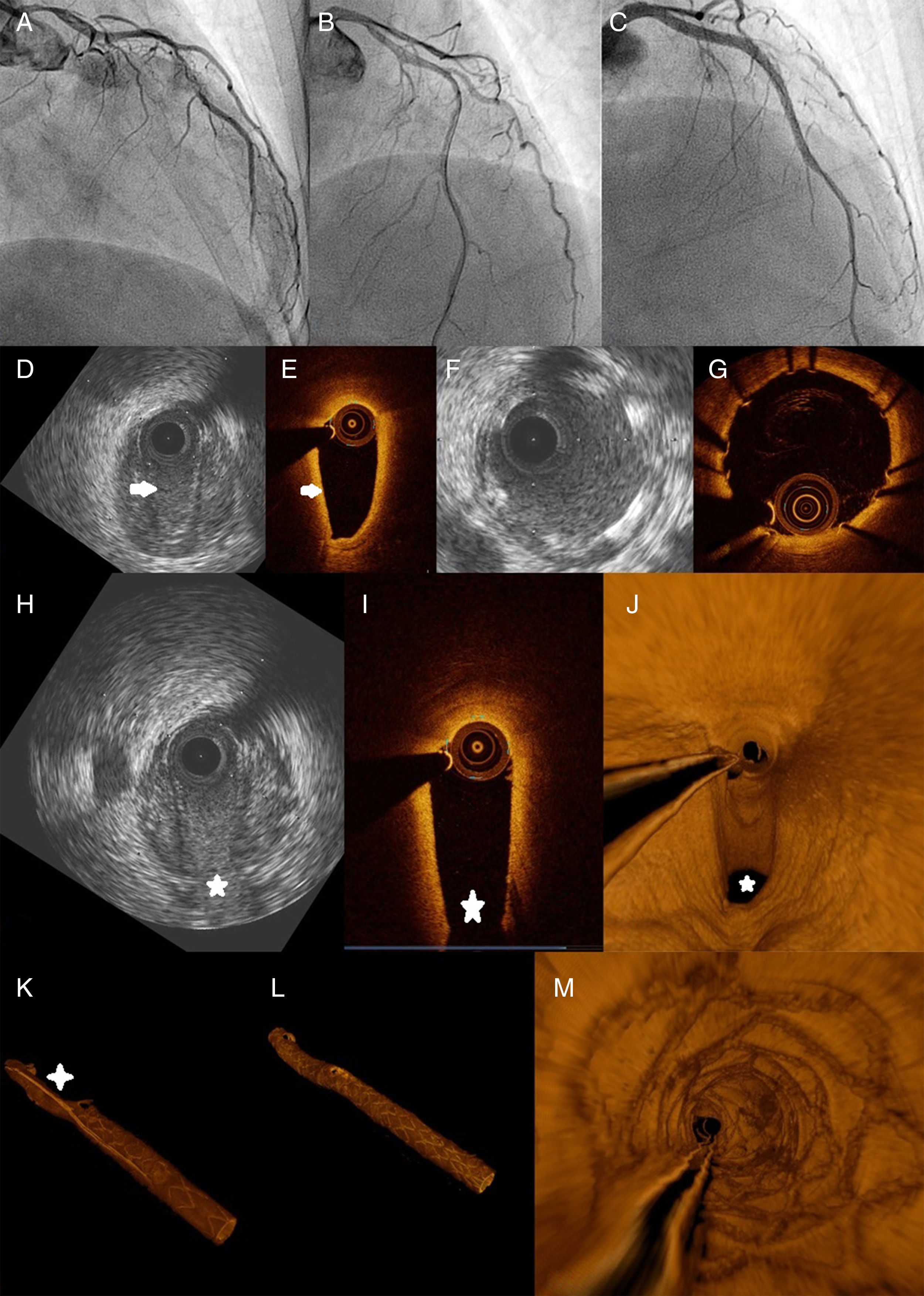
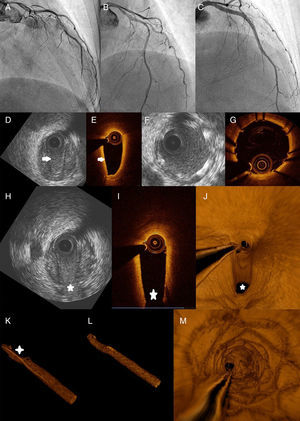
A 62-year-old woman was admitted with chest pain of two hours’ duration. Her medical history consisted only of dyslipidemia. The ECG presented changes (slight ST depression together with negative T waves) in the precordial leads, and the echocardiogram showed extensive and severe left ventricular anterolateral-apical hypokinesia (left ventricular ejection fraction 30%). Emergent catheterization was ordered, which showed severe left coronary flow disturbance (TIMI 1-2 flow) (Figure 1A; Video 1). An intra-aortic balloon pump (IABP) and a drug-eluting stent (DES) were implanted in the mid-distal left anterior descending artery (LAD) (Figure 1B). However, the flow disturbance persisted, with an apparent proximal stenosis on angiography. Optical coherence tomography (OCT) revealed diminished luminal area between the stent and the left main. Subsequent intravascular ultrasound (IVUS) provided a better view of the wall, showing an intracoronary hematoma (Figure 1D and E; Video 5), helping to establish the mechanism behind this situation.
(A-C) Coronary angiograms, cranial view: (A) at presentation, the flow is clearly diminished (TIMI 1-2); (B) after implantation of the first stent; (C) final angiographic result; (D and E) IVUS and OCT, respectively, of the mid segment of the left anterior descending artery. White arrows indicate the intimal flap; (F and G) IVUS and OCT, respectively, after stent implantation, showing correct expansion and apposition; (H and I) IVUS and OCT, respectively, displaying the hematoma at the origin of a patent septal branch (star); (J) three-dimensional (3-D) OCT reconstruction at the same level as (I); (K) 3-D reconstruction after implantation of the first stent. The cross shows the hematoma and the luminal compromise; (L and M) final 3-D result. IVUS: intravascular ultrasound; OCT: optical coherence tomography.
Spontaneous coronary dissection with intramural hematoma is a life-threatening condition of uncertain etiology and management. Conservative management is usually a good option if flow is preserved.1 Since our patient remained unstable, and suffered a propagation of the dissection, we decided to treat the remaining LAD/left main with two more DES, which was successful (Figure 1C, F, G and L; Videos 2 and 4). The patient progressed well and was successfully weaned from the IABP and discharged three days later. Peak troponin was 40 ng/dl (normal <0.05).
DiscussionIt is sometimes difficult to establish a definitive diagnosis by angiography only. The superior qualities of intracoronary imaging (IVUS and OCT) can help provide the correct diagnosis and guide management. In this critical patient, multimodality intracoronary imaging provided crucial data on the mechanism responsible and helped to optimize treatment. This case depicts a complex patient, with an uncommon condition (propagation of a dissection/hematoma). It also enables a direct comparison between the capabilities of OCT and IVUS, and indicates that IVUS, which has lower definition but deeper penetration, can have a key role in intracoronary diagnosis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of interestThe authors have no conflicts of interest to declare.