This study examined the efficacy of a brief inpatient psychoeducational intervention on knowledge about acute coronary syndromes (ACS), control of risk factors, and adaptive health habits and lifestyle. The intervention was intended to facilitate rehabilitation after ACS and its short- and medium-term impact was assessed.
MethodsOne hundred and twenty-one patients with ACS, admitted to a central cardiology unit in Portugal, were randomized to an experimental group (EG, n=65) or a control group (CG, n=56). We used the Portuguese versions of the Knowledge Questionnaire and the Health Habits Questionnaire. Patients were assessed at hospital admission, hospital discharge and one- and two-month follow-up.
ResultsThe intervention had a significant impact, increasing knowledge about ACS (F=500.834; p=0.000) in the EG, which was maintained at two-month follow-up, and changing health habits at two-month follow-up (F=218.129; p=0.000). The CG demonstrated decreased knowledge (F=3.368; p=0.069) during the same period.
ConclusionsA brief inpatient psychoeducational intervention has a positive effect on knowledge about ACS, risk factor control and promotion of positive health habits, and is effective in improving cardiac rehabilitation.
Este trabalho avaliou a eficácia de um programa de intervenção psicológica breve, na fase I da reabilitação cardíaca pós-síndroma coronária aguda (SCA), nos conhecimentos da doença e tratamento, controlo de fatores de risco e hábitos de saúde e estilo de vida. A intervenção foi realizada com vista a facilitar a reabilitação pós-SCA, tendo-se avaliado o impacto da mesma a curto e a médio prazo.
Material e métodosForam aleatorizados 121 doentes com SCA, admitidos na Unidade Coronária de um hospital central, num Grupo Experimental (GE, n = 65) e Grupo de Controlo (GC, n = 56). As versões portuguesas do Questionário de Conhecimentos acerca da Doença e Tratamento e do Questionário de Hábitos de Saúde avaliaram os conhecimentos acerca da doença e tratamento e os hábitos e estilo de vida. Os doentes foram avaliados na admissão e alta hospitalar bem como um e dois meses após a alta.
ResultadosVerificamos um aumento significativo dos conhecimentos sobre a SCA (F = 500,834; p = 0,000) no GE, o qual se manteve aos dois meses. Os resultados revelaram ainda efeitos significativos da intervenção na alteração dos hábitos de saúde no GE aos dois meses (F = 218,129; p = 0,000). O GC evidenciou uma diminuição do nível de conhecimentos (F = 3.368; p = 0,069) no mesmo período.
ConclusõesUma intervenção psicoeducativa breve aplicada no momento da hospitalização tem um efeito positivo no aumento do conhecimento sobre a SCA, controlo de fatores de risco e promoção de hábitos de saúde positivos, sendo eficaz na melhoria da reabilitação cardíaca.
As realization grows of the influence of psychological and behavioral factors on recovery from acute coronary syndrome (ACS), most current cardiac rehabilitation programs emphasize education about the disease and treatment as a way to improve treatment adherence and psychosocial adjustment.1–6
For recovery from ACS, psychoeducational interventions focus on education about disease and health while supporting the adoption of lifestyles appropriate to the needs of cardiac rehabilitation, optimization of risk factor control, and maintenance of protective factors.5,7-9 This approach emphasizes not only the active role that patients can play in their own recovery, but also the importance of a scientific approach to planning interventions designed to promote behavior changes that take into consideration an educational component throughout the rehabilitation process after ACS.2,10-12 Thus, key behavior changes include those affecting motivation, knowledge, the psychological and physical ability to perform the behavior, and the opportunity to perform it. Intervention strategies involving motivation should ensure that individuals have access to easily understandable information.13–17
It is well documented that education and promotion of knowledge about disease, risk factors and treatment during hospital stay have positive effects on the rehabilitation process after ACS and decrease cardiac vulnerability. Eshah et al.18 evaluated the effectiveness of a program of education, counseling and behavioral skills on knowledge, attitudes and beliefs about ACS and adoption of healthy lifestyles. The intervention group showed significantly better cardiac-related knowledge, and better scores for attitudes, health responsibility, nutritional behaviors, interpersonal relationships and adoption of healthy lifestyles. In the HUNT-2 study, the prevalence of low educational level was higher among those who developed acute myocardial infarction during the follow-up period.19 A study by Caspar-Bauguil et al.20 confirmed the positive impact of counseling and education about diet and lifestyle, conducted after ACS, on long-term outcome (one-year follow-up).
In summary, the results from clinical studies in this field are unanimous in emphasizing the importance of psychoeducation about the disease in cardiac rehabilitation after ACS, as well as identifying the period of hospital stay as a key time for effective preventive psychological intervention.2,5,21-24 The above findings highlight the importance of promoting planned interventions at the time of admission which provide education on cardiovascular risk factors, treatment and cardiac rehabilitation. The effectiveness of health education in cardiac rehabilitation can be enhanced if information is provided in the context of a planned and theoretically grounded intervention.2,5,11-17
MethodsStudy participants and designData were collected over a period of six months and a total of 208 patients were contacted. Of these, 47 refused to participate because of difficulty in traveling to the hospital to be assessed or inability to fill in the questionnaires. A further 26 patients had to leave the study due to cardiac surgery and 14 patients died.
The final study sample consisted of 121 patients (36 female and 85 male) diagnosed with ACS and admitted to the cardiology unit of a central hospital in Portugal. Mean age was 63.78 years (standard deviation 12.48) and 48% of the sample had ≤6 years of education. Informed consent was obtained from all participants included in the study, which was approved by the hospital's ethics committee.
Patients were randomized to an experimental group (EG; n=65) or a control group (CG; n=56) at the time of admission to the cardiology unit, using consecutive weekly randomization (e.g. week 1 for EG and week 2 for CG).25 Patients were assessed at four time points: hospital admission – pre-test (T1), hospital discharge – post-test (T2), one-month follow-up (T3) and two-month follow-up (T4).
An intervention was administered to the EG within 2-3 days of hospital admission, consisting of two sessions (1 hour 15 min each) and a follow-up session (20 min) one month after hospital discharge. The intervention modality was in group format (mean of six participants per group) and included health education about ACS and cardiac rehabilitation (session 1) and promotion of psychosocial adjustment rehabilitation after ACS (session 2). Session 3 was a follow-up session one month post-discharge and focused on reviewing previous commitments, identifying successes and challenges, promoting goal reformulation and discussing future implementation strategies.
The main research question predicted a significant effect of the intervention on the psychosocial variables studied (disease knowledge and health habits) with better outcomes for EG than for CG.
InstrumentsThe instruments used were the Portuguese versions of the Knowledge Questionnaire and the Health Habits Questionnaire26 (Supplementary Material). The two instruments have similar psychometric properties to the original scales. The Knowledge Questionnaire consists of 19 statements that assess knowledge regarding ACS and its treatment. The Health Habits Questionnaire consists of seven multiple-choice questions assessing diet (consumption of fats and salt), consumption of other substances (coffee, alcohol and tobacco), and health behaviors (exercise and frequency of blood pressure measurement). An overall risk behavior index (RBI) was calculated by coding responses indicating negative habits (risk behaviors) as 1 and responses indicating positive habits as 0. The sum of these responses gave the RBI. This was calculated at only two time points, pre-test (T1) and at follow-up two months after discharge (T3). This was because, while in hospital, patients have no control over the items that were assessed, and it thus makes no sense to assess changes in this situation.
Statistical analysisStatistical analyses were conducted using IBM SPSS version 19.0. Univariate and multivariate repeated measures were used to test the effect of the intervention. Age and pre-test values of the outcome variables were entered as covariates. The equivalence of the experimental and control groups at pre-test, in terms of demographic and psychosocial variables, was established using group comparison statistics (chi-square test for nominal variables and t test for continuous variables).
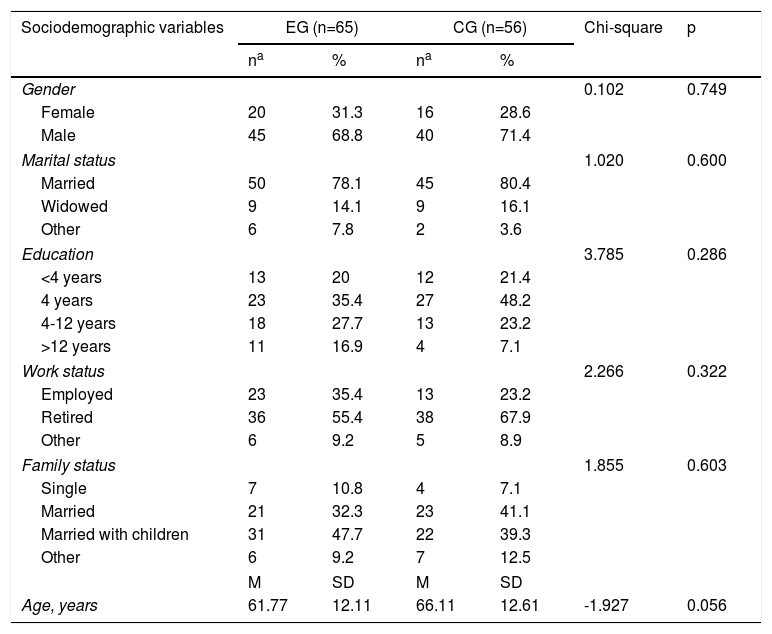
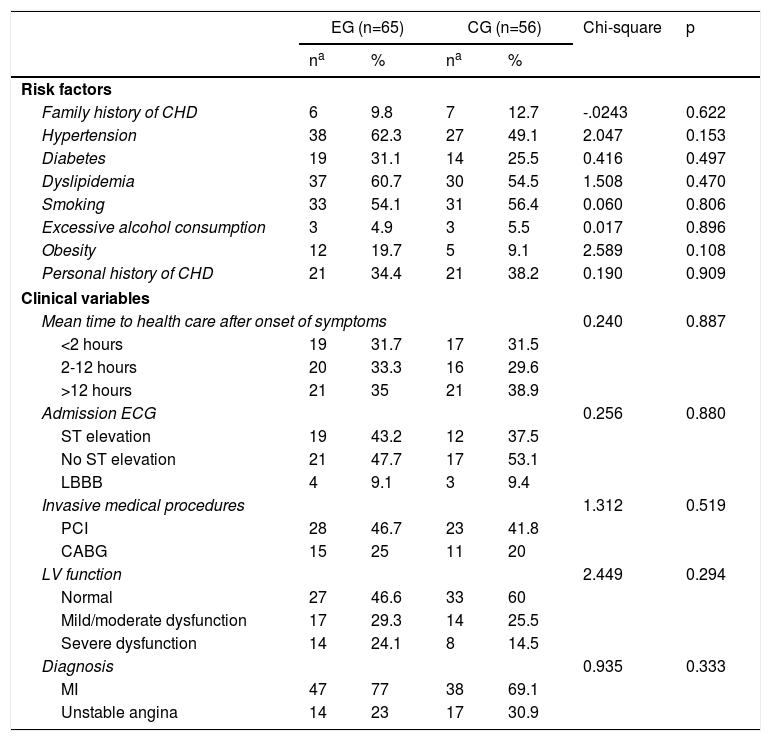
ResultsTables 1 and 2 present the sociodemographic and clinical characteristics of the study sample. The groups were equivalent in most sociodemographic variables and all clinical variables, with only a marginally significant difference found for age, the CG being slightly older (66.1±12.6 vs. 61.8±12.1 years).
Sociodemographic characteristics of the study sample and comparison by intervention group.
| Sociodemographic variables | EG (n=65) | CG (n=56) | Chi-square | p | ||
|---|---|---|---|---|---|---|
| na | % | na | % | |||
| Gender | 0.102 | 0.749 | ||||
| Female | 20 | 31.3 | 16 | 28.6 | ||
| Male | 45 | 68.8 | 40 | 71.4 | ||
| Marital status | 1.020 | 0.600 | ||||
| Married | 50 | 78.1 | 45 | 80.4 | ||
| Widowed | 9 | 14.1 | 9 | 16.1 | ||
| Other | 6 | 7.8 | 2 | 3.6 | ||
| Education | 3.785 | 0.286 | ||||
| <4 years | 13 | 20 | 12 | 21.4 | ||
| 4 years | 23 | 35.4 | 27 | 48.2 | ||
| 4-12 years | 18 | 27.7 | 13 | 23.2 | ||
| >12 years | 11 | 16.9 | 4 | 7.1 | ||
| Work status | 2.266 | 0.322 | ||||
| Employed | 23 | 35.4 | 13 | 23.2 | ||
| Retired | 36 | 55.4 | 38 | 67.9 | ||
| Other | 6 | 9.2 | 5 | 8.9 | ||
| Family status | 1.855 | 0.603 | ||||
| Single | 7 | 10.8 | 4 | 7.1 | ||
| Married | 21 | 32.3 | 23 | 41.1 | ||
| Married with children | 31 | 47.7 | 22 | 39.3 | ||
| Other | 6 | 9.2 | 7 | 12.5 | ||
| M | SD | M | SD | |||
| Age, years | 61.77 | 12.11 | 66.11 | 12.61 | -1.927 | 0.056 |
CG: control group; EG: experimental group; M: mean; SD: standard deviation.
Clinical characteristics of the study sample and comparison by intervention group.
| EG (n=65) | CG (n=56) | Chi-square | p | |||
|---|---|---|---|---|---|---|
| na | % | na | % | |||
| Risk factors | ||||||
| Family history of CHD | 6 | 9.8 | 7 | 12.7 | -.0243 | 0.622 |
| Hypertension | 38 | 62.3 | 27 | 49.1 | 2.047 | 0.153 |
| Diabetes | 19 | 31.1 | 14 | 25.5 | 0.416 | 0.497 |
| Dyslipidemia | 37 | 60.7 | 30 | 54.5 | 1.508 | 0.470 |
| Smoking | 33 | 54.1 | 31 | 56.4 | 0.060 | 0.806 |
| Excessive alcohol consumption | 3 | 4.9 | 3 | 5.5 | 0.017 | 0.896 |
| Obesity | 12 | 19.7 | 5 | 9.1 | 2.589 | 0.108 |
| Personal history of CHD | 21 | 34.4 | 21 | 38.2 | 0.190 | 0.909 |
| Clinical variables | ||||||
| Mean time to health care after onset of symptoms | 0.240 | 0.887 | ||||
| <2 hours | 19 | 31.7 | 17 | 31.5 | ||
| 2-12 hours | 20 | 33.3 | 16 | 29.6 | ||
| >12 hours | 21 | 35 | 21 | 38.9 | ||
| Admission ECG | 0.256 | 0.880 | ||||
| ST elevation | 19 | 43.2 | 12 | 37.5 | ||
| No ST elevation | 21 | 47.7 | 17 | 53.1 | ||
| LBBB | 4 | 9.1 | 3 | 9.4 | ||
| Invasive medical procedures | 1.312 | 0.519 | ||||
| PCI | 28 | 46.7 | 23 | 41.8 | ||
| CABG | 15 | 25 | 11 | 20 | ||
| LV function | 2.449 | 0.294 | ||||
| Normal | 27 | 46.6 | 33 | 60 | ||
| Mild/moderate dysfunction | 17 | 29.3 | 14 | 25.5 | ||
| Severe dysfunction | 14 | 24.1 | 8 | 14.5 | ||
| Diagnosis | 0.935 | 0.333 | ||||
| MI | 47 | 77 | 38 | 69.1 | ||
| Unstable angina | 14 | 23 | 17 | 30.9 | ||
CABG: coronary artery bypass grafting; CHD: coronary heart disease; ECG: electrocardiogram; LBBB: left bundle branch block; LV: left ventricular; MI: myocardial infarction; PCI: percutaneous coronary intervention.
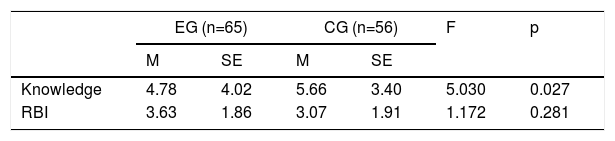
The EG and CG differed at pre-test in disease knowledge (Table 3), with higher levels in the CG (5.66±3.40 vs. 4.78±4.02) (F=5.030; p=0.027), although this difference was controlled for in hypothesis testing. The groups were similar regarding health habits (Table 3), with a mean of 3.63 for risk behavior in the EG and 3.7 in the CG (F=1.17, p=0.281).
Results of analysis of covariance for knowledge (Knowledge Questionnaire) and overall risk behavior index (Health Habits Questionnaire) at pre-test, with group as factor, controlling for age (n=121).
| EG (n=65) | CG (n=56) | F | p | |||
|---|---|---|---|---|---|---|
| M | SE | M | SE | |||
| Knowledge | 4.78 | 4.02 | 5.66 | 3.40 | 5.030 | 0.027 |
| RBI | 3.63 | 1.86 | 3.07 | 1.91 | 1.172 | 0.281 |
CG: control group; EG: experimental group; M: mean; SE: standard error.
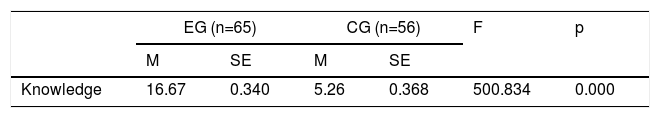
The results of analysis of covariance and repeated multivariate analysis of covariance at post-test and during follow-up demonstrated the significant impact of the psychoeducational intervention in increasing knowledge about the disease and treatment. At post-test, the EG had a significantly higher level of knowledge (mean 16.67) than the CG (mean 5.26) (F=500.834; p=0.000) (Table 4). This difference is even more significant considering that the EG presented a lower level of knowledge about the disease and treatment at pre-test.
Results of analysis of covariance for knowledge about the disease and its treatment (Knowledge Questionnaire) at post-test, with group as factor, controlling for age and the respective pre-test subscales (n=121).
| EG (n=65) | CG (n=56) | F | p | |||
|---|---|---|---|---|---|---|
| M | SE | M | SE | |||
| Knowledge | 16.67 | 0.340 | 5.26 | 0.368 | 500.834 | 0.000 |
CG: control group; EG: experimental group; M: mean; SE: standard error.
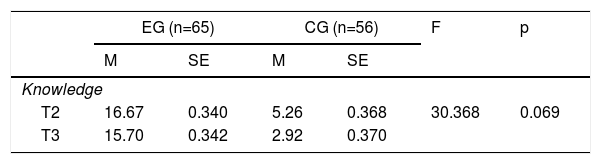
The EG maintained their greater knowledge in the two-month period after hospital discharge (mean 17.70), unlike the CG, which tended to show even less knowledge than they had previously had (mean 2.92) (F=3.368; p=0.069) (Table 5).
Results of multivariate analysis of covariance for knowledge about the disease and its treatment (Knowledge Questionnaire), using time and group as factors and controlling for age and the respective pre-test subscales (n=121).
| EG (n=65) | CG (n=56) | F | p | |||
|---|---|---|---|---|---|---|
| M | SE | M | SE | |||
| Knowledge | ||||||
| T2 | 16.67 | 0.340 | 5.26 | 0.368 | 30.368 | 0.069 |
| T3 | 15.70 | 0.342 | 2.92 | 0.370 | ||
CG: control group; EG: experimental group; M: mean; SE: standard error; T2: post-test; T3: 2-month follow-up.
Thus, over time there was a significant difference between EG and CG profiles. In the EG, there was a marked increase in knowledge from pre- to post-test and two-month follow-up (mean T1=4.78, mean T3=15.70), indicating that the gains of the intervention were maintained during the post-hospitalization period. In the CG, the low level of knowledge persisted from pre- (mean 5.66) to post-test (mean 5.26), and tended to decrease further at two months (mean 2.92).
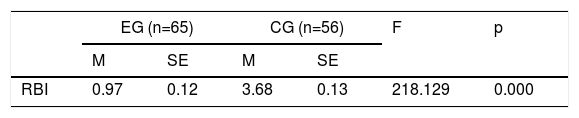
Health habitsAnalysis of the results obtained indicates positive progress over time regarding health habits in the EG, but not in the CG. In the two-month follow-up period, the CG presented a higher RBI (mean 3.68) than the EG (mean 0.97), with a statistically significant difference (p=0.000) (Table 6).
Results of analysis of covariance for the overall risk behavior index (Health Habits Questionnaire) in the two-month follow-up period, using group as factor and controlling for age and risk behavior at pre-test (n=121).
| EG (n=65) | CG (n=56) | F | p | |||
|---|---|---|---|---|---|---|
| M | SE | M | SE | |||
| RBI | 0.97 | 0.12 | 3.68 | 0.13 | 218.129 | 0.000 |
Higher risk behavior index values indicate greater risk behavior. Health habits were assessed at only two time points: at pre-test and at two-month follow-up.
CG: control group; EG: experimental group; M: mean; RBI: risk behavior index; SE: standard error.
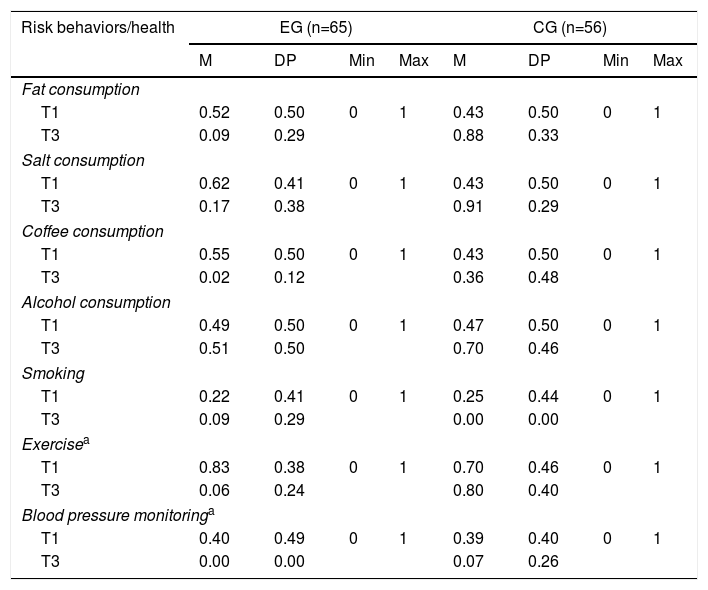
Analyzing the descriptive data which constitute the RBI at pre-test and post-test, it can be observed that, over time, the EG presented a significant decrease in risk behavior, such as consumption of fat and salt, as well as improvement in health habits such as regular exercise and blood pressure monitoring (Table 7).
Descriptive analysis of items of the Health Habits Questionnaire by group at pre-test and two-month follow-up (n=121).
| Risk behaviors/health | EG (n=65) | CG (n=56) | ||||||
|---|---|---|---|---|---|---|---|---|
| M | DP | Min | Max | M | DP | Min | Max | |
| Fat consumption | ||||||||
| T1 | 0.52 | 0.50 | 0 | 1 | 0.43 | 0.50 | 0 | 1 |
| T3 | 0.09 | 0.29 | 0.88 | 0.33 | ||||
| Salt consumption | ||||||||
| T1 | 0.62 | 0.41 | 0 | 1 | 0.43 | 0.50 | 0 | 1 |
| T3 | 0.17 | 0.38 | 0.91 | 0.29 | ||||
| Coffee consumption | ||||||||
| T1 | 0.55 | 0.50 | 0 | 1 | 0.43 | 0.50 | 0 | 1 |
| T3 | 0.02 | 0.12 | 0.36 | 0.48 | ||||
| Alcohol consumption | ||||||||
| T1 | 0.49 | 0.50 | 0 | 1 | 0.47 | 0.50 | 0 | 1 |
| T3 | 0.51 | 0.50 | 0.70 | 0.46 | ||||
| Smoking | ||||||||
| T1 | 0.22 | 0.41 | 0 | 1 | 0.25 | 0.44 | 0 | 1 |
| T3 | 0.09 | 0.29 | 0.00 | 0.00 | ||||
| Exercisea | ||||||||
| T1 | 0.83 | 0.38 | 0 | 1 | 0.70 | 0.46 | 0 | 1 |
| T3 | 0.06 | 0.24 | 0.80 | 0.40 | ||||
| Blood pressure monitoringa | ||||||||
| T1 | 0.40 | 0.49 | 0 | 1 | 0.39 | 0.40 | 0 | 1 |
| T3 | 0.00 | 0.00 | 0.07 | 0.26 | ||||
CG: control group; EG: experimental group; Max: maximum; Min: minimum; T1: pre-test; T3: two-month follow-up.
Our results demonstrate the short- and medium-term effectiveness of the intervention program developed and assessed in this study, indicating a positive effect on important aspects of rehabilitation after ACS, such as increase in knowledge about the disease and treatment, and improvement in health habits. These results are clinically significant and have important implications for the literature on the planning and assessment of the effectiveness of psychological interventions in cardiac rehabilitation. As stated above, education and the promotion of knowledge regarding the disease, risk factors, and treatment are pivotal to the quality of the process of cardiac rehabilitation.5,8,17 In our study, the provision of information about the disease, conducted in the context of the intervention program, was associated with improvements in health habits and lifestyles. Similarly to other studies in this area,2,19,24 our results illustrate the usefulness of a scientific approach in planning interventions that promote behavior change and the importance of the educational component throughout the rehabilitation process after ACS.
The level of knowledge regarding the disease and treatment increased significantly in the EG from pre- to post-test, but not in the CG, in whom there was no significant change. This result is particularly striking because the EG had a lower level of knowledge about the disease and treatment (e.g. knowledge about the symptoms and consequences of the disease) at pre-test than the CG. This significant increase in the level of knowledge in the EG thus confirms the importance of education about the disease, treatment and rehabilitation in terms of the effectiveness of psychological intervention in this area.
As predicted, there was an increase in health-promoting behaviors and a decrease in risk behaviors from pre- to post-test in the EG. These positive changes were not found in the CG. Regarding health habits, statistically significant differences were recorded between the two groups from pre- to post-test, with improvements for the EG: over time (between hospital admission and two months after discharge), the EG significantly decreased risk behaviors, such as consumption of fats and salt, and increased positive habits such as regular exercise and blood pressure monitoring. The intervention thus had a positive effect on three important areas of cardiac rehabilitation: nutrition (decreased consumption of fats and salt), physical activity (significant increase in regular exercise) and adherence to preventive therapeutic measures (increased frequency of blood pressure measurement). The detrimental effects of high cholesterol and salt intake and hypertension on the severity of coronary atherosclerosis are well known.27,28 At the same time, exercise is essential for cardiovascular health and physical rehabilitation after ACS, which is why it is a key target of current cardiac rehabilitation programs.15,21,28
In our study, there was a slight difference in age at pre-test, with the EG being slightly younger than the CG (p=0.56), which may have impacted our results. Younger age is considered to be one of the strongest predictors of drop-out from cardiac rehabilitation programs,12,29 and models which combine education and intervention are needed to promote motivation and adherence in these patients. Longer psychological intervention programs after hospital discharge, which combine education on the disease and cognitive-behavioral intervention, might be a good alternative, as suggested in a previous study by our group.30 In the present study, the randomization process did not include age or gender, and we chose a generic model of intervention (not specific for gender or age). The fact that men and women present different psychosocial profiles regarding response and adaptation to ACS, and therefore require different interventions, has been reported in the literature,26 and highlights the importance of gender-specific intervention protocols in cardiac rehabilitation regarding emotional and behavioral aspects. There has also been reference to the impact of age in post-ACS rehabilitation, with older women having a worse psychosocial profile. Therefore, taking into consideration the importance of variables such as age and gender in psychosocial outcomes, the impact of age should be further investigated in future studies and taken into account when planning intervention programs.
It is important to put these gains into context with those that were observed in emotional state and disease cognition in our earlier study,22 particularly the significant decrease in anxiety levels and depression that the EG revealed from hospital admission to the post-intervention time point, as well as the acquisition of more adaptive disease cognition. These gains were not seen in the CG, which highlights the effectiveness of the psychological intervention program tested. In light of this, the biopsychosocial intervention we performed appears to have had a synergistic effect involving several psychosocial dimensions associated with rehabilitation, which supports the use of multifaceted approaches in this type of intervention.
In recent years we have investigated the effectiveness of various modalities of psychological intervention in cardiac rehabilitation.30–32 In our experience, the hospitalization period provides a unique opportunity for effective intervention regarding both psychosocial prevention and education.33 Other authors have reported that brief educational interventions during the hospitalization period are effective in improving adherence to healthy behaviors15 and improving disease perceptions.34,35 The fact that patients are close to the acute event, are in a controlled environment where the intervention is available, and have the free time to participate, provides a window of opportunity for intervention. In our study, as well as positive results in disease perceptions, the EG showed increased knowledge about disease and treatment, less anxiety and depression over time, and positive changes in health habits and lifestyle at two months after the intervention. The post-discharge session may have had an important role in relapse prevention and competence reinforcement.
In conclusion, the intervention we used appears to have promoted a profile of adjustment over time, helping patients in the EG to deal more appropriately with the implications of the rehabilitation process. By contrast, patients in the CG experienced a significant decrease in their level of knowledge and cardiovascular health-promoting behaviors over time. In addition, the results of our study support the idea that the hospitalization period provides a unique opportunity for preventive psychosocial intervention and that psychological factors at this stage can play a key role in the rehabilitation process. The study's results are particularly interesting considering that the intervention administered was brief (of less than three hours duration) with a low associated cost. The follow-up plan for the present study includes a medium- and long-term follow-up (up to one year) to investigate whether the positive results are consistent and sustained in the long term. However, in our opinion, the results obtained so far clearly indicate the benefits of integrating a psychological intervention in phase I of hospital cardiac rehabilitation programs.
Ethical approvalAll procedures in this study were in accordance with the standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflicts of interestThe authors have no conflicts of interest to declare.