The authors present the case of a 34-year-old male patient seen in our department due to palpitations. On the electrocardiogram monomorphic ventricular tachycardia (VT) was documented, treated successfully with amiodarone. The subsequent study revealed a normal echocardiogram and an apical aneurysm of the left ventricle on magnetic resonance imaging, confirmed by computed tomography coronary angiography that also excluded coronary disease.
He underwent an electrophysiological study to determine the origin of the VT and to perform catheter ablation using electroanatomical mapping. VT was induced and radiofrequency applications were performed in the left ventricular aneurysm area. VT was no longer inducible, with acute success. Despite this it was decided to implant a subcutaneous implantable cardioverter-defibrillator (ICD). Eight months after the ablation the patient was admitted again due to VT, treated by the ICD.
Os autores apresentam o caso de um doente do sexo masculino, com 34 anos de idade, que recorreu ao serviço de urgência por palpitações. No eletrocardiograma inicial foi documentada uma taquicardia ventricular (TV) monomórfica. O estudo subsequente revelou um ecocardiograma sem alterações, tendo sido observado um aneurisma apical do ventrículo esquerdo na ressonância magnética cardíaca e confirmado na angiografia coronária por tomografia computorizada que excluiu doença coronária.
O doente foi submetido a estudo eletrofisiológico com o objetivo de ser determinada a origem da TV e realizar ablação por cateter recorrendo a mapeamento eletroanatómico. Foi possível induzir TV e efetuar aplicações de radiofrequência na área do aneurisma do ventrículo esquerdo. No final do procedimento a TV deixou de ser induzível. Apesar do sucesso agudo, foi decidido implantar um cardioversor desfibrilhador subcutâneo. Aos oito meses após ablação, o doente foi novamente admitido em internamento por TV, tratada com choques de CDI.
Congenital left ventricular aneurysm (LVA) was first described in 1816.1 It is a rare cardiac malformation, defined as a protrusion from the ventricular cavity with a wide connection (ratio of the connection to the body of the anomaly >1) and without contractility, which may present with an akinetic or dyskinetic movement during systole.2 Ohlow et al.3 reported the prevalence of congenital left ventricular aneurysms and diverticulum as 0.76% in a coronary angiogram population.
According to a recent review congenital left ventricular aneurysms are asymptomatic in 41.8% of patients,4 but can be associated with heart failure, arrhythmias, systemic embolization and sudden death due to ventricular rupture.2,5
Ventricular tachycardia may be present in 18.4% of patients with LVA,5 but few data are available concerning these patients’ clinical outcome. Treatment of ventricular tachycardia (VT) in patients with congenital aneurysms can be difficult, and surgical and electrophysiological strategies have been described.6–8
Our case documents a rare case of monomorphic VT in a young patient with a congenital left ventricular apical aneurysm, diagnosed by a multimodality imaging study, and our treatment options.
Case reportA 34-year-old male, a regular sports player, presented to our department due to palpitations that had started while playing tennis. He had a past history of Hodgkin lymphoma treated by chemotherapy eight years before, with no evidence of recurring disease.
Previous to the documented episode the patient described two episodes of self-limited palpitations, the first four years previously while playing table tennis, and another eight weeks before the described episode during an argument. He had no family history of sudden death, syncope, ventricular arrhythmias or cardiomyopathy.
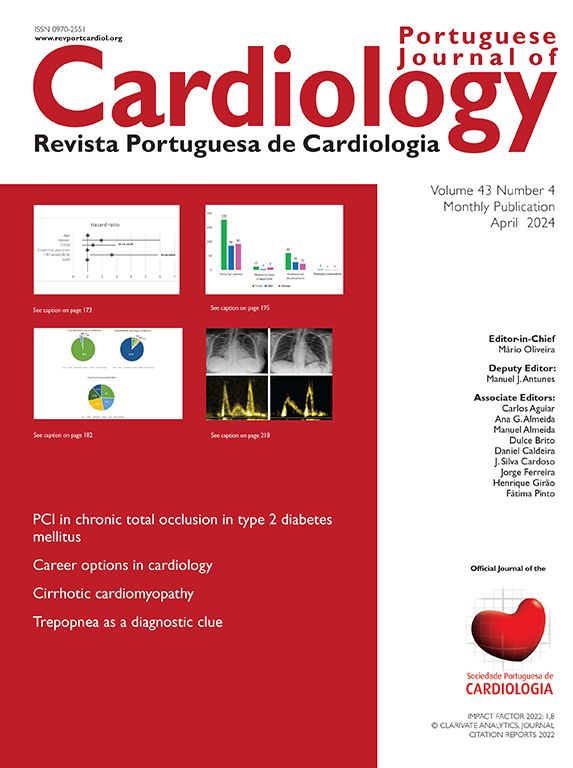
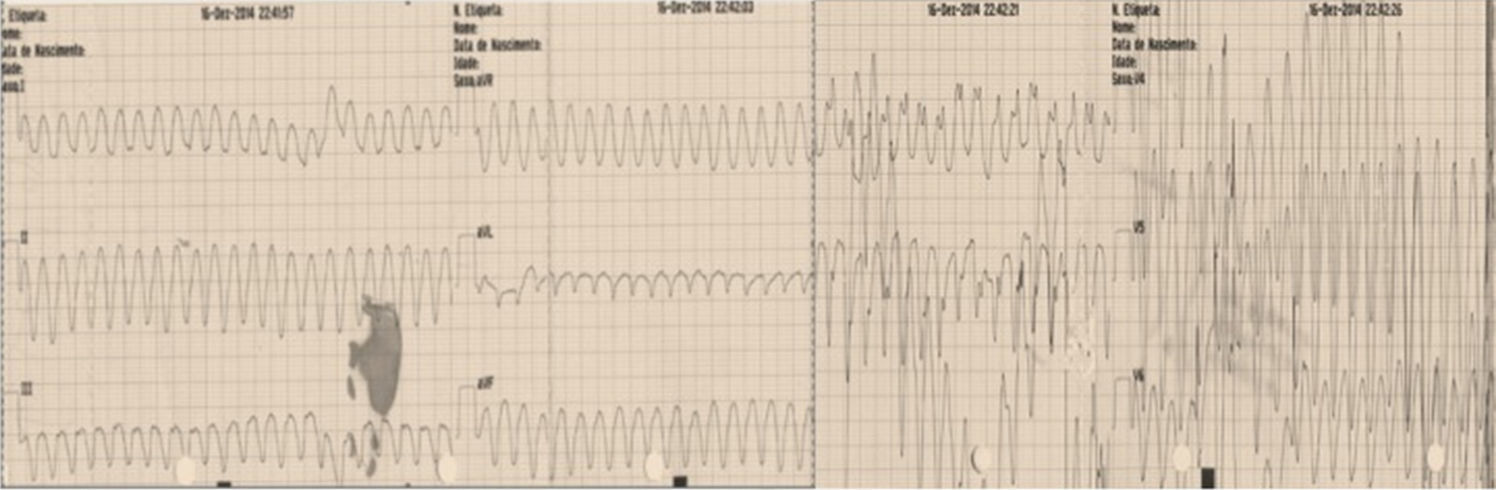
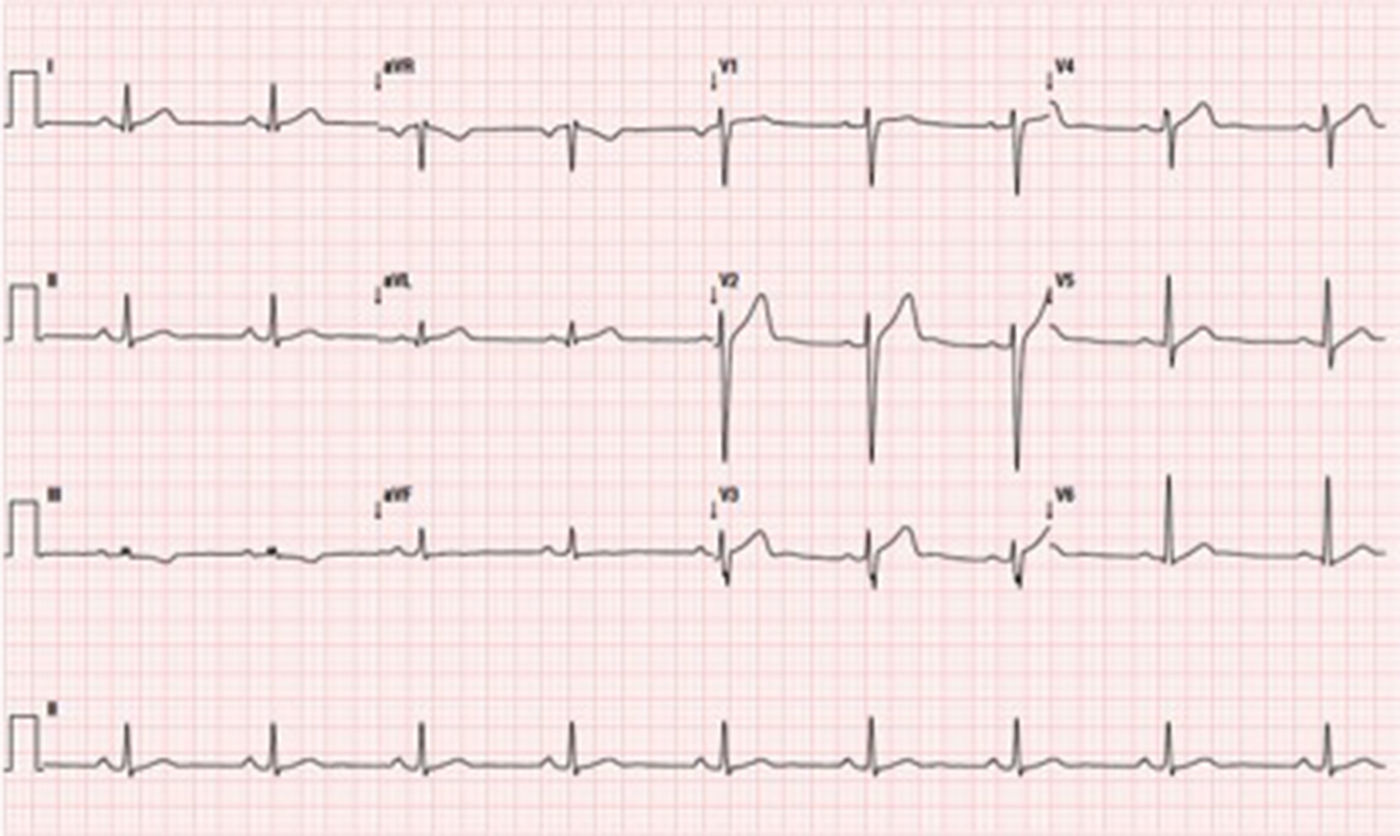
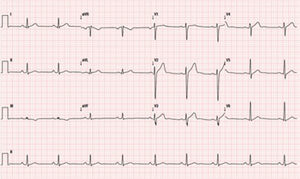
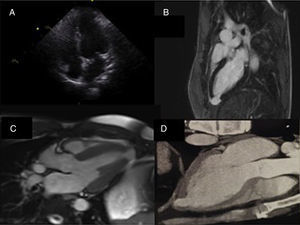
On the day that he presented to our department an electrocardiogram (ECG) was performed (Figure 1), which revealed monomorphic ventricular tachycardia with right bundle branch block morphology and superior axis, with a ventricular rate of 256 bpm. As the patient was stable, amiodarone infusion was started, achieving sinus rhythm. His ECG in sinus rhythm showed no changes (Figure 2). The echocardiogram (Figure 3A) revealed no structural abnormalities and the physical examination and laboratory tests showed no remarkable findings.
Multimodality imaging of the left ventricular apical aneurysm. (A) Echocardiogram, 4-chamber view, showing no remarkable changes; (B) cardiac magnetic resonance imaging with late gadolinium enhancement depicting myocardial delayed enhancement restricted to the wall of the left ventricular apical aneurysm; (C) cardiac magnetic resonance imaging at end-systole demonstrating the lack of systolic thickening of the left ventricular apical aneurysm wall; (D) computed tomography image of the left ventricle clearly showing the thinning of the left ventricular aneurysm wall compared to the surrounding myocardium.
In order to exclude structural cardiac abnormalities it was decided to perform cardiac magnetic resonance imaging (Figure 3B and C) that exhibited a left ventricular apical aneurysm: “a saccular apical formation with a thin wall on late gadolinium enhancement, without any scarring of the surrounding myocardium”. He underwent computed tomography coronary angiography that excluded coronary disease and described the same left ventricular apical formation (Figure 3D).
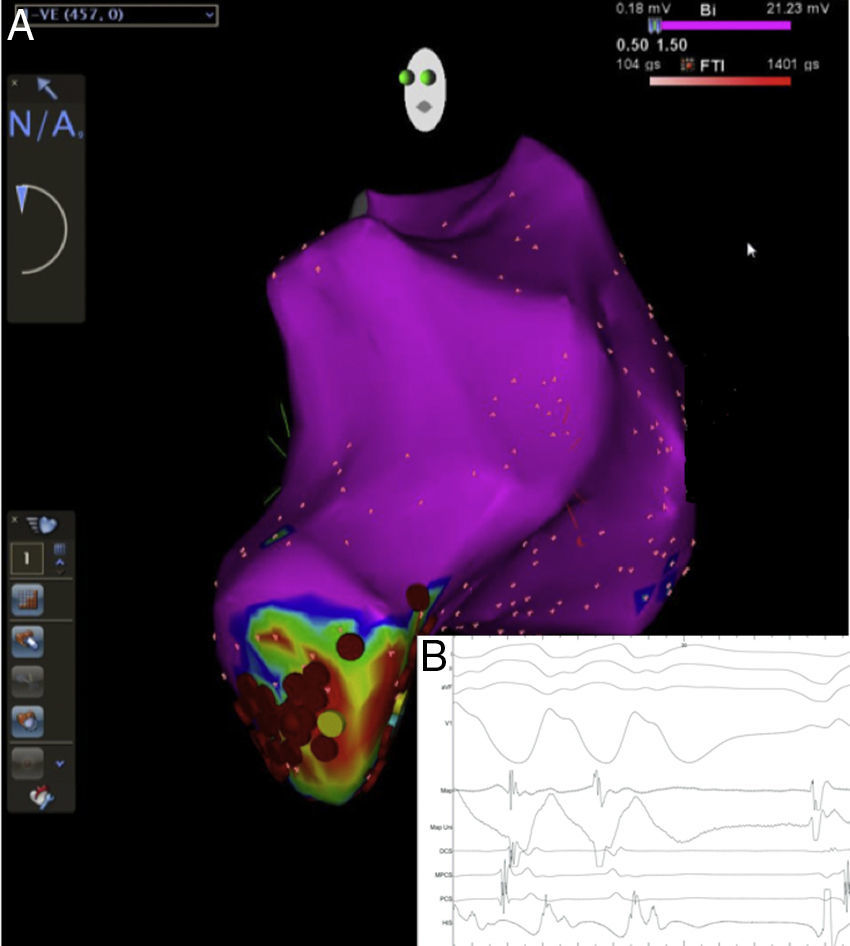
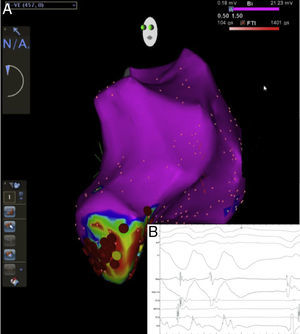
After the diagnosis it was decided to perform an electrophysiological study to determine the origin of the VT and to perform catheter ablation. It was possible to induce VT similar to the clinical VT during the electrophysiological study, and electroanatomical mapping was performed (Figure 4). The reentry circuit and exit point of the tachycardia were inside the aneurysm. Radiofrequency applications were performed with an open-irrigated ablation catheter, targeting diastolic potentials during VT, the tachycardia being terminated during applications. Additional radiofrequency applications were performed in sinus rhythm targeting the exit point of the clinical VT with pace mapping. Radiofrequency applications were limited to 30 W, with a total time of 7 min. At the end of the procedure VT was no longer inducible. Despite this success, it was decided to place a subcutaneous implantable cardioverter-defibrillator (ICD).
(A) Three-dimensional electroanatomic image of the left ventricle acquired during electrophysiological study. It can be seen that the ventricular tachycardia was localized to the apical aneurysm and the radiofrequency applications; (B) diastolic potentials at the ablation catheter (MAP), and interruption of ventricular tachycardia during radiofrequency applications.
Eight months after the ablation procedure the patient presented to the emergency department complaining of ICD shocks, due to ventricular tachycardia. He was put on amiodarone 100 mg and bisoprolol 5 mg once daily. The amiodarone dosage was increased and the possibility of performing an aneurysm resection or a reablation procedure was discussed with the patient.
DiscussionDiagnosis and treatment of VT are often a challenge. This case describes a patient with a left ventricular apical aneurysm with no coronary disease, and late gadolinium enhancement on the aneurysm wall suggesting a fibrotic wall. Fibrotic apical congenital aneurysms have been described previously, being the most probable diagnosis in this case.4 Radiofrequency ablation was the treatment selected for this patient's VT. Successful use of this technique was reported by Haegeli et al. in two of three patients.9 ICD implantation is recommended in patients with VT and structural cardiac abnormalities, and so, despite the good acute result of radiofrequency ablation in this case, a subcutaneous ICD was implanted. This choice was made considering that this was a young patient who had undergone VT ablation and that recurrence of ventricular arrhythmias was likely. However, the question arises whether the advantages of a subcutaneous device in a young patient, particularly the lower risk of long-term complications related to intravascular lead complications,10 outweigh the benefits of antitachycardia pacing with a conventional ICD. Our patient was symptom-free for eight months after the ablation and then needed two appropriate ICD shocks due to VT.
As surgical resection of ventricular aneurysms has been described, with good results, as an alternative treatment for patients with recurrent symptoms, we are considering this option for this patient.4
The authors consider this case relevant due to the rarity of the condition and because there are few cases described in the literature of patients treated with electrophysiological study and ICD implantation. To our knowledge this is the first case in which a subcutaneous ICD was implanted. There is a lack of evidence concerning the management of congenital LVA and more data are needed in this field.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interestThe authors have no conflicts of interest to declare.