The follow-up of patients with atrial fibrillation (AF) presents an opportunity to alert patients and their families on how to recognize and act in the event of stroke. Our aim was to compare stroke recognition-to-door time and prehospital stroke code activation in patients with known AF (KAF) and AF detected after stroke (AFDAS).
MethodsWe performed a retrospective cohort study of consecutive patients receiving acute recanalization treatment for acute ischemic stroke between January 2016 and August 2022, with AF as a potential stroke cause. Patients were divided into KAF and AFDAS, and stroke recognition-to-door time and prehospital stroke code activation were compared. In the KAF subgroup, we assessed whether the use of preadmission anticoagulation was associated with the studied prehospital parameters.
ResultsWe included 438 patients, 290 female (66.2%), mean age 79.3±9.4 years. In total, 238 patients had KAF (54.3%) and 200 (45.7%) had AFDAS. Of those with KAF, 114 (48.1%) were pretreated with anticoagulation. Patients with KAF and AFDAS had no differences in stroke recognition-to-door time (74.0 [55.0–101.0] vs. 78.0 [60.0–112.0] min; p=0.097) or prehospital stroke code activation [148 (64.6%) vs. 128 (65.3%); p=0.965]. In the KAF subgroup, preadmission anticoagulation did not influence stroke recognition-to-door time or mode of hospital admission.
ConclusionStroke recognition-to-door time and prehospital stroke code activation were similar between patients with known or newly diagnosed AF. Preadmission anticoagulation treatment also did not affect the studied parameters. Our findings highlight a missed opportunity to promote stroke knowledge in patients followed due to AF.
O seguimento de doentes com fibrilhação auricular (FA) constitui uma oportunidade para alertar doentes e famílias sobre como reconhecer e atuar perante um Acidente Vascular Cerebral (AVC). O nosso objetivo foi comparar o tempo reconhecimento-admissão e modo de admissão hospitalar [ativação de Via Verde AVC (VV-AVC) extra-hospitalar] entre doentes com FA conhecida (FAC) e de novo (FAN).
MetodologiaEstudo de coorte retrospetivo de doentes consecutivos com AVC isquémico agudo, submetidos a terapêutica de recanalização, entre janeiro de 2016 e agosto 2022, com FA como potencial causa do AVC. Os doentes foram divididos em FAC e FAN e compararam-se os tempos reconhecimento-admissão hospitalar e ativação de VV-AVC extra-hospitalar. No subgrupo de doentes com FAC, analisamos a influência de terapêutica prévia com anticoagulação nos mesmos parâmetros pré-hospitalares.
ResultadosIncluímos 438 doentes, 290 (66,2%) do sexo feminino, com média de idade de 79,3±9,4 anos; 238 (54,3%) doentes com FAC e 200 (45,7%) com FAN. No grupo de doentes com FAC, 114 (48,1%) encontravam-se sob anticoagulação. Não houve diferenças no tempo reconhecimento-admissão (74,0 [55,0–101,0] versus 78,0 [60,0–112,0]; p = 0,097), nem na ativação de VV-AVC extra-hospitalar [148(64,6%) versus 128(65,3%); p = 0,965]. No subgrupo de doentes com FAC, anticoagulação prévia não teve influência nos mesmo indicadores pré-hospitalares.
ConclusãoO tempo reconhecimento-admissão e ativação de VV-AVC extra-hospitalar foram semelhantes entre doentes com FAC e FAN. A realização prévia de anticoagulação não modificou estes resultados. Os nossos resultados salientam uma potencial oportunidade perdida para promoção de educação sobre AVC em doentes seguidos em consulta por FA.
Atrial fibrillation (AF) is the most common arrhythmia in adults worldwide and an important risk factor for ischemic stroke (IS). It is estimated that 20% of all strokes are due to AF, with some studies showing increasing numbers in the last few years.1 In Portugal, stroke is the leading cause of death and disability,2 and AF is highly prevalent, particularly in individuals over 65 years old.3,4
The key acute recanalization treatments for IS are intravenous thrombolysis and mechanical thrombectomy, which have been demonstrated to improve patients’ outcomes.5,6 In both, treatment indication and effect are time-dependent, with a shorter time from stroke onset to recanalization associated with better outcomes.5,7
Delay in seeking medical attention after the onset of stroke symptoms is an important reason for the underuse of acute recanalization therapies, and a significant percentage of patients with stroke do not activate emergency medical services.8 Patients’ or witnesses’ knowledge of stroke, including stroke symptoms and available treatments, seems to reduce prehospital delays.9,10
In this context, stroke education campaigns aimed at improving early recognition of and rapid response to the symptoms of stroke by patients and witnesses are crucial to increasing access to treatment and ultimately improving patient outcomes. Since in many cases broad-based campaigns have been successful in raising stroke awareness, but have had little effect on actual behavior in response to stroke,10 more targeted intervention, directed toward high-risk patients and their family members, could be an alternative approach.
The follow-up of patients with AF presents a vital opportunity to alert patients and families on how to recognize stroke and what to do when one occurs, aiming to reduce the time to hospital admission and reperfusion treatment.
With this study, we aimed to compare stroke recognition-to-door time and prehospital stroke code activation in patients with known AF (KAF) and in those with AF detected after stroke (AFDAS).
MethodsStudy design, patient selection and study variablesThis was a retrospective cohort study of consecutive IS patients receiving acute recanalization treatment in our hospital between January 2016 and August 2022, and with AF defined as stroke cause. Patients with in-hospital stroke were excluded.
We collected demographic data (age and gender), previous modified Rankin Scale (mRS), vascular risk factors (hypertension, coronary heart disease, diabetes, dyslipidemia, smoking, heart failure, previous IS or transient ischemic attack [TIA]), stroke location (anterior vs. posterior circulation), and stroke characteristics (severity at admission as assessed by the National Institutes of Health Stroke Scale [NIHSS], presence of aphasia, presence of extinction/inattention, and whether stroke onset was witnessed).
We reviewed stroke recognition-to-door time and type of stroke code activation (prehospital vs. at hospital admission). Stroke recognition-to-door time corresponds to either: (1) stroke onset-to-hospital admission if patients or bystanders were able to report the time of initial stroke symptoms or (2) found-to-hospital admission if the stroke was unwitnessed and the patient was unable to report the time of initial stroke symptoms.
Patients were divided into two groups according to the timing of AF diagnosis: (1) KAF, if AF was diagnosed before the stroke event or (2) AFDAS, when AF was diagnosed during stroke admission or during the first three months of follow-up. Preadmission use of anticoagulation was also collected, including all patients receiving any type of anticoagulant therapy, regardless of appropriate dosing or compliance.
Statistical analysisDescriptive data were expressed as mean (standard deviation) or median (interquartile range) for continuous variables and frequency (percentage) for dichotomous variables. Comparisons between KFA and AFDAS were made using the chi-square test, Fisher's exact test, Student's t test, or Mann–Whitney U test, as appropriate. In the KAF subgroup, we also assessed whether the use of preadmission anticoagulation was associated with the same studied prehospital parameters (stroke recognition-to-door time and prehospital stroke code activation). The significance level was set at p≤0.05. The statistical analysis was performed with R version 4.2.1 (R Foundation for Statistical Computing, Vienna, Austria).
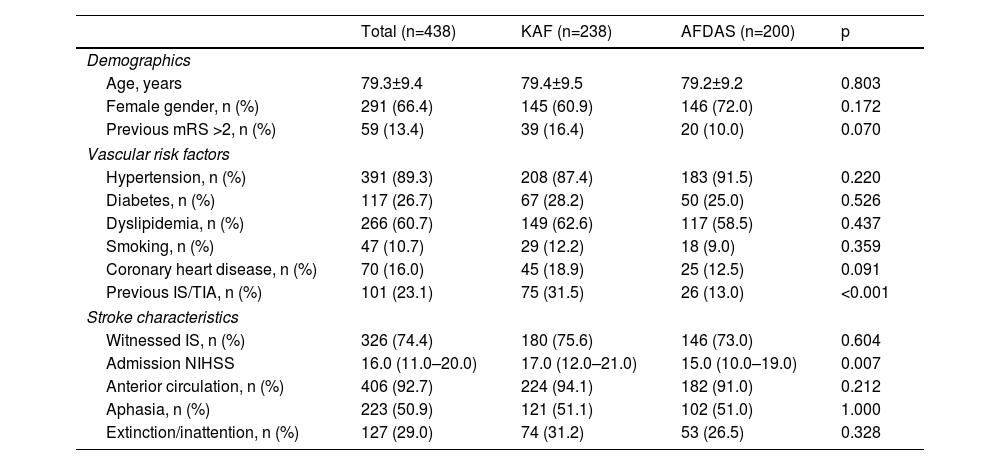
ResultsThe study included 438 patients, 290 female (66.2%), with a mean age of 79.3±9.4 years. In total, 238 (54.3%) patients had KAF and 200 (45.7%) had AFDAS. Patients with KAF had a higher prevalence of heart failure (83 [34.9%] vs. 30 [15.0%]; p<0.001) and previous IS or TIA (75 [31.5%] vs. 26 [13.0%]; p<0.001), and higher NIHSS (17.0 [12.0–21.0] vs. 15.0 [10.0–19.0]; p=0.007). No other differences between groups in baseline or stroke characteristics were recorded (Table 1).
Comparison of baseline and stroke characteristics between patients with known atrial fibrillation and atrial fibrillation detected after stroke.
| Total (n=438) | KAF (n=238) | AFDAS (n=200) | p | |
|---|---|---|---|---|
| Demographics | ||||
| Age, years | 79.3±9.4 | 79.4±9.5 | 79.2±9.2 | 0.803 |
| Female gender, n (%) | 291 (66.4) | 145 (60.9) | 146 (72.0) | 0.172 |
| Previous mRS >2, n (%) | 59 (13.4) | 39 (16.4) | 20 (10.0) | 0.070 |
| Vascular risk factors | ||||
| Hypertension, n (%) | 391 (89.3) | 208 (87.4) | 183 (91.5) | 0.220 |
| Diabetes, n (%) | 117 (26.7) | 67 (28.2) | 50 (25.0) | 0.526 |
| Dyslipidemia, n (%) | 266 (60.7) | 149 (62.6) | 117 (58.5) | 0.437 |
| Smoking, n (%) | 47 (10.7) | 29 (12.2) | 18 (9.0) | 0.359 |
| Coronary heart disease, n (%) | 70 (16.0) | 45 (18.9) | 25 (12.5) | 0.091 |
| Previous IS/TIA, n (%) | 101 (23.1) | 75 (31.5) | 26 (13.0) | <0.001 |
| Stroke characteristics | ||||
| Witnessed IS, n (%) | 326 (74.4) | 180 (75.6) | 146 (73.0) | 0.604 |
| Admission NIHSS | 16.0 (11.0–20.0) | 17.0 (12.0–21.0) | 15.0 (10.0–19.0) | 0.007 |
| Anterior circulation, n (%) | 406 (92.7) | 224 (94.1) | 182 (91.0) | 0.212 |
| Aphasia, n (%) | 223 (50.9) | 121 (51.1) | 102 (51.0) | 1.000 |
| Extinction/inattention, n (%) | 127 (29.0) | 74 (31.2) | 53 (26.5) | 0.328 |
AFDAS: atrial fibrillation diagnosed after stroke; IS: ischemic stroke; KAF: known atrial fibrillation; mRS: modified Rankin Scale; NIHSS: National Institutes of Health Stroke Scale; TIA: transient ischemic attack.
There were no differences between patients with KAF and AFDAS in stroke recognition-to-door time (74.0 [55.0–101.0] vs. 78.0 [60.0–112.0] min, p=0.097) or prehospital stroke code activation (148 [64.6%] vs. 128 [65.3%], p=0.965).
In patients with KAF, 114 (48.1%) were under anticoagulation at stroke onset. Preadmission anticoagulation was not associated with stroke recognition-to-door time (72.0 [55.0; 92.0] vs. 78.0 [51.8; 103.8] min, p=0.446) or prehospital stroke code activation (76 [65.0%] vs. 72 [64.3%], p=1.000).
DiscussionIn our study, patients with KAF did not have different stroke recognition-to-door times or different rates of prehospital stroke code activation from patients with AFDAS. In the subgroup of patients with KAF, preadmission anticoagulation was not associated with the same prehospital parameters.
As stated, patients’ and bystanders’ stroke knowledge are key to avoiding failure to identify stroke symptoms and delays in activating emergency medical services, which ultimately can contribute to lower recanalization treatment rates and worse outcomes. Significant prehospital delays in patients with ischemic stroke were recently documented in Portugal.11
In the general population, stroke knowledge is poor,12,13 with previous studies showing that a low percentage of patients contact the emergency medical services within an hour of stroke onset and less than half recognize stroke as the cause of their symptoms.14,15 Different strategies have been designed to improve stroke knowledge, and while general and broad-based campaigns had inconsistent outcomes, interventions targeted at specific subgroups such as children or high-risk stroke populations have shown more consistent results.16,17
Because patients with AF are at high risk for stroke and have regular medical follow-up visits (such as anticoagulation prescription and treatment of AF symptoms or other comorbidities), our hypothesis was that these patients and their family members could be more aware of stroke symptoms and what to do in the event of stroke than those without AF. This knowledge would translate into prompt stroke recognition, activation of emergency medical services, and timely hospital admissions. The same rationale was considered for preadmission anticoagulation in patients with KAF – anticoagulation use could be considered as a surrogate for more regular medical follow-up, in contrast to those not under this therapy.
Contrary to our hypothesis, having KAF or treatment with anticoagulation were not associated with better prehospital parameters. This could mean that a window of opportunity to educate high-risk patients about stroke in follow-up visits is being missed.
Previous studies report conflicting data on the association between AF diagnosis and time to hospital admission but do not specify whether AF was previously known or newly diagnosed.9,18,19 As previously reported,20–22 patients with KAF had a higher prevalence of previous stroke and greater deficits at admission, which are known to be associated with earlier hospital arrival,18,19 and theoretically could also have contributed to shorter admission times in patients with KAF.
Our study has limitations. Due to its retrospective design, registration bias cannot be excluded. Since this study was based on our institutional acute stroke treatment registry, patients not receiving intravenous thrombolysis or mechanical thrombectomy were not included, which could have influenced our results. Delays in hospital admission and prehospital stroke code activation were used as a surrogate for patients’ stroke knowledge but could have been influenced by other factors, such as other medical comorbidities, distance to a hospital at stroke onset, and performance of prehospital health professionals. The inclusion of patients in only one hospital, with a stable catchment area, and no changes in prehospital pathways over the study period should have helped to circumvent most of these limitations. Even if patients are well informed about stroke symptoms and what to do in the event of stroke, if they become severely disabled, they will be unable to contact emergency medical services. In such cases, the knowledge of family members or other bystanders will be key. The education level of patients and bystanders was not assessed, and this could potentially have influenced the results. Additionally, cognitive performance among patients with previous stroke, which may also have impacted the time to contact emergency medical services, was also not assessed. Of note, in our study, the percentages of patients with aphasia or inattention, as well as of witnessed stroke, did not differ between groups. Also, having KAF does not necessarily translate into routine medical visits, just as the opposite does not imply their absence. By comparing patients with KAF and AFDAS our goal was to analyze patients with a similar demographic and vascular risk profile that could translate into similar medical outpatient needs aside from AF. With differences only in the prevalence of previous IS/TIA and heart failure, the two groups were relatively well balanced in terms of vascular risk profile. Similar limitations can be considered for preadmission anticoagulation. Patients with AF may occasionally have contraindications that require suspension of anticoagulation, or more often, acute medical complications or interventions that require temporary anticoagulation interruption.
Medical consultations are an opportunity for physicians to educate patients about stroke risk and families about how to identify stroke symptoms and how to act when they occur. Our results show an opportunity gap for stroke-related education for patients with KAF.
As recommended, cardiologists, neurologists, internists, family physicians, and others, should not neglect their role in patient education, and should promote stroke knowledge, when possible, in both primary and secondary prevention.23
ConclusionIn our study, a previous diagnosis of atrial fibrillation and preadmission anticoagulation for stroke prevention were not associated with stroke recognition-to-door time or prehospital stroke code activation rate. Our study shows a potential missed opportunity to promote stroke knowledge in patients attending medical appointments due to atrial fibrillation.
Conflicts of interestThe authors have no conflicts of interest to declare.